Endoscopic management of anastomotic stricture after living-donor liver transplantation
Article information
Abstract
The most effective and fundamental treatment for end-stage liver disease is liver transplantation. Deceased-donor liver transplantation has been performed for many of these cases. However, living-donor liver transplantation (LDLT) has emerged as an alternative because it enables timely procurement of the donor organ. The success rate of LDLT has been improved by development of the surgical technique, use of immunosuppressant drugs, and accumulation of post-transplantation care experience. However, the occurrence of biliary stricture after LDLT remains a problem. This article reviews the pathogenesis, diagnosis, endoscopic management, and long-term outcomes of post-liver transplantation biliary stricture, with a focus on anastomotic stricture.
INTRODUCTION
Liver transplantation (LT) is a revolutionary treatment for patients with acute liver failure or end-stage liver disease, and it prolongs survival and allows for full recovery [1,2]. LT can be divided into deceased-donor and living-donor LT (DDLT and LDLT, respectively) according to the organ delivery method [3]. In Western countries, where social systems are well established to enable a smooth process of organ procurement from deceased donors, DDLT is the preferred procedure. In Eastern countries, where organ procurement systems are not well established and still developing, LDLT is more common [4,5].
The management of complications occurring after LT is very important for the patient and graft survival. Patients with complications post-LT may experience frequent hospitalization, increased treatment costs, and, rarely, liver failure. Biliary stricture is the most common (approximately 40%) biliary complication occurring after LT [6,7]. The incidence of biliary stricture is approximately 5% after DDLT and approximately 24% and 60% for left and right lobe grafts, respectively, after LDLT [8-10].
This article provides an overview of the pathogenesis, diagnosis, endoscopic management, and long-term outcomes of post-LT biliary stricture, with a focus on anastomotic stricture (AS).
PATHOGENESIS OF BILIARY STRICTURE
Bile duct epithelium is more vulnerable to ischemic damage compared with hepatocytes and the vascular endothelium. Such damage is a major cause of the development of biliary stricture after LT [11]. In addition, differences in the diameter between donor and recipient bile ducts are often large, and AS can occur frequently, depending on the surgeon’s skill and experience with duct-to-duct anastomosis in LDLT [12].
CLASSIFICATION OF BILIARY STRICTURES
Biliary strictures occurring after LT can be anastomotic or non-anastomotic, with approximately 80% being AS [13]. ASs are usually isolated, localized (within 5 mm) to the anastomosis site, and formed over short ductal lengths [14]. Non-anastomotic strictures (NASs) account for approximately 10% to 25% of post-LT biliary strictures. Unlike ASs, they often develop at multiple sites and over greater lengths [15-17].
RISK FACTORS FOR BILIARY STRICTURE
Established risk factors for AS include the operator’s low technical proficiency, a large difference between donor and recipient bile duct diameters, excessive anastomotic tension, frequent use of electrocautery for hemostasis, and concomitant infection [18-22]. Risk factors for NAS include hepatic artery injury or thrombosis, reversible bile duct fibrosis caused by prolonged ischemia, blood type incompatibility, and use of vasopressin in donors [18,23]. In rare cases, hepatitis C and cytomegalovirus may also be risk factors for NAS [24,25].
CLINICAL MANIFESTATIONS
Post-LDLT biliary stricture is often accompanied by symptoms of obstructive jaundice, such as dark urine and pruritus. However, it is often asymptomatic. As most LT recipients take immunosuppressant drugs and/or show hepatic denervation, they rarely complain of abdominal pain, even when biliary stricture occurs [26-28].
LABORATORY EVALUATION
Abnormalities on liver function tests, such as altered serum transaminase, bilirubin, alkaline phosphatase, and/or gamma-glutamyl transferase levels, are often found in patients with biliary stricture. However, such abnormalities can also reflect acute or chronic rejection, reactivation of underlying viral hepatitis, or drug-induced hepatitis. To determine the most appropriate treatment, further evaluation must be performed to confirm that abnormalities on liver function tests are caused by biliary stricture [12].
IMAGING EVALUATION
Ultrasonography
Ultrasonography (USG) i s a non-invasive imaging modality that enables observation of the intrahepatic bile ducts and confirmation of the surrounding vascular patency. However, USG is not suitable for confirmation of the presence of biliary stricture. Sharma et al. [29] reported that only 38% to 66% of biliary strictures occurring after LT are diagnosed successfully by USG. Therefore, diagnosis and screening for biliary stricture cannot be performed using USG alone.
Computed tomography
In recent years, multidetector computed tomography (CT) has been developed, and its resolution has improved. As a result, CT is used widely as a follow-up examination for patients after LT. It is also useful for the identification of non-biliary complications, such as fluid collection around the operation site. However, the utility of contrast-enhanced CT may be limited by the occurrence of adverse events related to the intravenously administered contrast agent [12]. Thus, development of a more stable and safer contrast agent is needed.
Magnetic resonance cholangiography
Magnetic resonance cholangiography (MRC) can be used to obtain detailed images of the whole biliary tract, and its sensitivity and specificity for the diagnosis of AS are both ≥ 90% [30,31]. In addition, the performance of unnecessary interventions can be reduced due to the high negative predictive value of MRC findings [32]. Thus, detailed observation of the biliary tract by MRC not only increases the success rate of interventions to treat biliary stricture but also reduces intervention-related complications. However, MRC has no therapeutic capability and is expensive.
Hepatobiliary scintigraphy
Hepatobiliary scintigraphy using 99m-technetium-labeled iminodiacetic acid has shown excellent accuracy for the diagnosis of bile leaks. However, studies have yielded inconsistent findings regarding its performance in the diagnosis of biliary stricture. Some authors have reported that the sensitivity and specificity of scintigraphy for the diagnosis of post-LT biliary stricture were 75% and 100%, respectively, whereas others have reported a sensitivity of only 60% [33,34]. These results suggest that the use of this imaging modality for the diagnosis of post-LT biliary stricture cannot be strongly recommended [35,36].
ENDOSCOPIC MANAGEMENT OF BILIARY STRICTURE
Overview
Biliary reconstruction in LDLT has been achieved using Roux-en-Y hepaticojejunostomy. In recent years, however, duct-to-duct anastomosis has been used in most cases. As a result, endoscopic management is feasible and can be attempted as first-line therapy for biliary stenosis occurring after LDLT [37,38]. New endoscopic accessories have been developed and endoscopic techniques improved during the past two decades, increasing the success rate of endoscopic management [39]. When NAS occurs post-LDLT, endoscopic management at all affected duct sites is practically impossible. Therefore, endoscopic management should be performed preferentially in patients with AS.
Conventional endoscopic management protocol
In general, selective cannulation of the bile duct is performed as in endoscopic retrograde cholangiography (ERC), and a guidewire is passed to the proximal side of the AS. Next, endoscopic sphincterotomy is performed. Subsequently, balloon dilation is used at the stricture site, and the AS is expanded using a Sohendra biliary dilation catheter or Sohendra stent retriever, as needed. Finally, a plastic stent is inserted into the stricture site. After 2 to 3 months, the stent is replaced by a stent of larger diameter [40-42].
Need for balloon dilatation
Balloon dilation is commonly used before insertion of a plastic stent into a stricture site. However, some endoscopists prefer to insert the stent directly, without dilation, in the first ERC procedure, and to use balloon dilation during the second ERC procedure, prior to stent exchange [12]. No study has shown that this method results in a better outcome compared with the conventional protocol, and further research is needed.
Need for endoscopic sphincterotomy
Endoscopic sphincterotomy may prevent post-ERC pancreatitis due to the blockage of pancreatic juice after the insertion of a plastic stent of large diameter [40]. However, the function of the sphincter of Oddi is lost irreversibly after this procedure, potentially resulting in duodenobiliary reflux, stent occlusion, and bacterial colonization in the biliary system [43-47]. For this reason, sphincterotomy may reduce the advantage of biliary reconstruction with duct-to-duct anastomosis in patients undergoing LDLT.
Recently, Isayama et al. [46] described the “inside stent method” for AS management. In this method, a plastic stent is placed across the AS without performing sphincterotomy, and the distal tip of the stent is positioned inside the bile duct. Using this method, Isayama et al. [46] inserted stents into the desired locations in 80% of 118 patients with post-LDLT AS and confirmed stricture resolution in 69% of the patients.
The performance of sphincterotomy may reduce the overall procedure time, as it facilitates the use of accessories and cannulation in subsequent ERC procedures. A prospective randomized controlled trial comparing the “inside stent method” with the conventional protocol is needed to establish the efficacy of this approach.
Ideal treatment interval
When stent exchange is performed every 2 to 3 months, according to the conventional protocol, approximately 1 year is needed to resolve an AS [22,47-51]. Therefore, several attempts have been made to shorten the duration of treatment.
Morelli et al. [52] performed stent exchange every 2 weeks, with a mean treatment duration of 3.6 months and a high (87%) success rate. In another study, stents with maximal diameters were inserted during the initial ERC procedure, and stent exchange was used only when stent occlusion occurred [53]. Neither of these studies involved follow-up of a large number of patients, and these methods cannot yet be recommended as standards of care.
Use of self-expanding metal stents
Because self-expanding metal stents (SEMSs) have larger diameters (up to 30 Fr) than those of plastic stents, their use is expected to achieve excellent resolution of various benign biliary strictures, including post-LDLT AS [54]. When uncovered SEMSs are used, occlusion due to the ingrowth of granulation tissue and other complications, such as pseudoaneurysm in surrounding vascular strictures, may occur [54-57]. The use of fully covered SEMSs (cSEMSs) can overcome these drawbacks but may result in occlusion of secondary branches of the bile duct and subsequent bile stasis [58]. In addition, cSEMSs have a migration rate of 16% to 33%, resulting in failure to expand the AS for a sufficient period of time and an increased number of ERC procedures [59,60]. In a recent study involving the use of a new cSEMS (Kaffes stent, Taewoong Medical, Seoul, Korea) with a central waist, a high treatment success rate (83%) and low migration rate (6%) were achieved [61]. Furthermore, the Kaffes stent can be moved into the endoscopy channel by grasping and pulling of the lasso (Fig. 1).
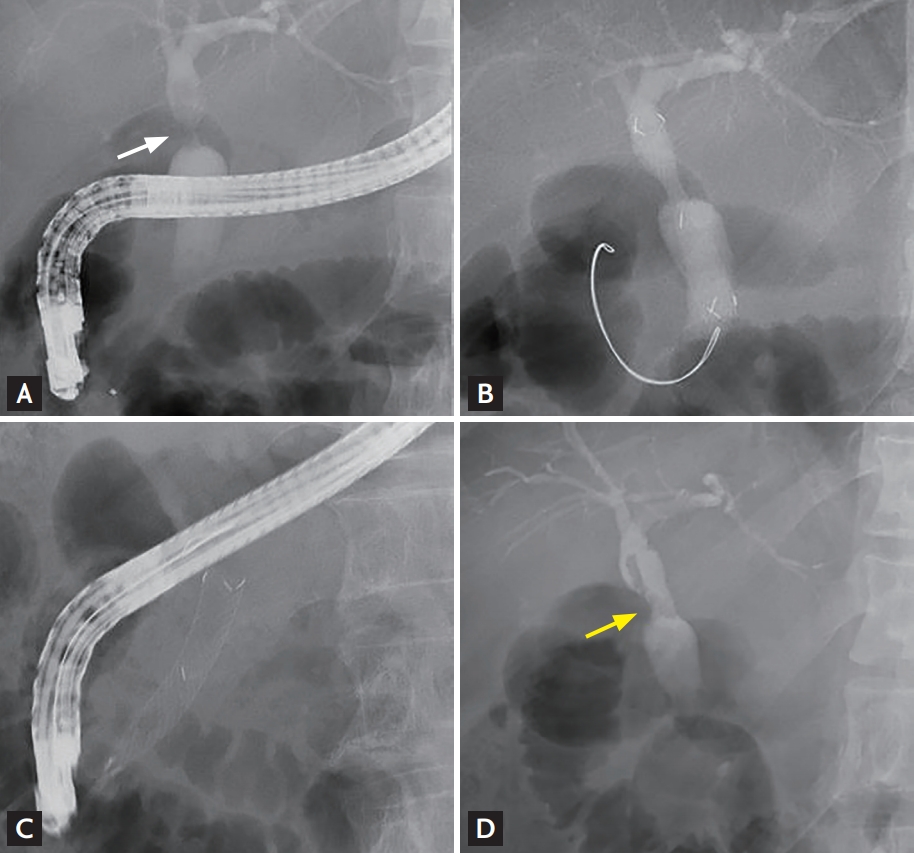
Endoscopic management of a biliary anastomotic stricture (AS) using a fully covered self-expanding metal stent. (A) Cholangiography revealed the presence of a biliary AS (white arrow) after living-donor liver transplantation. (B) A fully covered self-expanding metal stent was placed across the AS. (C) Three months later, the metal stent was removed successfully through the duodenoscopy channel by pulling of the lasso. (D) Resolution of the AS (yellow arrow) was observed.
Long-term outcomes
The incidence of stricture recurrence during long-term follow-up after AS treatment using the conventional protocol is 12% to 30% (Table 1) [15,62-65]. However, the use of ERC to treat AS was introduced relatively recently, and longer-term follow-up studies are needed. In addition, existing studies have been criticized due to the heterogeneity of parameters such as donor age and endoscopic management protocols. Thus, no generalization can be made about the long-term outcomes of AS treatment post-LDLT.
Overall survival after LDLT with or without AS
Several studies have shown that the occurrence of AS after LDLT does not affect overall survival [62,66]. Recently, Chok et al. [67] reported that the 1-, 3-, and 5-year survival rates did not differ between patients with AS (n = 55) and those without AS (n = 210; 97.3% vs. 91.4%, 90% vs. 85.3%, and 84.5% vs. 82.5%, respectively; p = 0.574).
CONCLUSIONS
LDLT is a fundamental treatment for patients with end-stage liver disease that can cure the disease without the need to wait for a deceased donor. The success rate of LDLT has been improved greatly by development of the surgical technique, use of immunosuppressant drugs, and accumulated experience in postoperative care. However, the occurrence of AS after LDLT remains a problem. In recent years, biliary reconstruction with duct-to-duct anastomosis has been performed, and ASs have been treated with ERC. Several new treatment protocols designed to ensure higher treatment success rates with shorter treatment durations have been developed. In the future, studies examining the use of diverse, novel endoscopic accessories and stents are expected.
Notes
No potential conflict of interest relevant to this article was reported.
