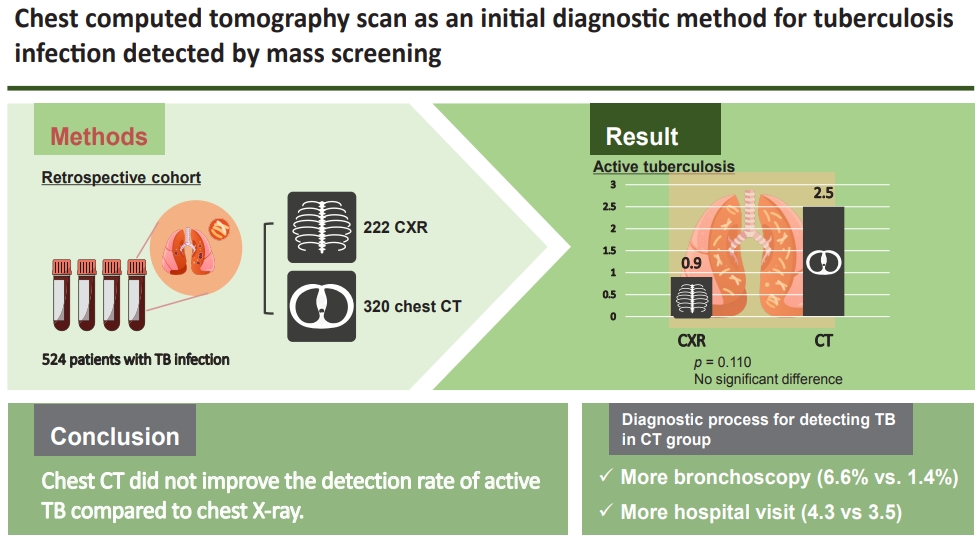
Chest computed tomography scan as an initial diagnostic method for tuberculosis infection detected by mass screening
Article information
Abstract
Background/Aims
We assessed the diagnostic yield of chest computed tomography (CT) as an initial diagnostic method for patients with a tuberculosis (TB) infection detected by mass screening in a country with an intermediate TB burden.
Methods
A retrospective study was conducted on patients with TB infection detected by mass screening performed between January 2015 and March 2018. The patients were classified according to whether they had a chest X-ray (CXR) or CT scan as an initial diagnostic test to exclude active TB.
Results
Of 542 patients with TB infection detected by mass screening, 222 and 320 were initially examined by CXR and CT, respectively; the two modalities showed no significant difference in rate of detection of patients with active TB (0.9% and 2.5%, respectively; p = 0.110). However, chest CT was associated with further invasive tests using bronchoscopy and respiratory specimens, and significantly increased the frequency of hospital visits.
Conclusions
Chest CT was not supported as an initial diagnostic method to rule out active TB in patients with a TB infection detected by mass screening in a country with an intermediate TB burden.
INTRODUCTION
Pulmonary tuberculosis (TB) is a major infectious disease worldwide, with high morbidity and mortality [1]. One of the main strategies to prevent new TB infections is to treat latent TB infection (LTBI), to prevent the progression from TB infection to active disease [2]. In South Korea, country with an intermediate TB burden of an incidence rate of 70 TB patients per 100,000 people in 2018, TB contact investigations in facilities for treating TB are being enhanced as part of a wider project to control the disease; epidemiological studies are also being conducted [1,3–5]. Considering the possibility of a major outbreak of TB affecting vulnerable persons, mass screening was conducted in medical institutions, postpartum care centers, daycare centers, and social welfare facilities since 2017 in South Korea [6].
When subjects are diagnosed with a TB infection by an LTBI test, such as the tuberculin skin test (TST) or interferon gamma release assay (IGRA), it is important to first exclude active TB; LTBI is ultimately diagnosed after confirming that there is no evidence of active TB. Diagnosis based on symptoms and chest X-ray (CXR) findings is currently recommended [7]. H owever, while many studies have reported a low yield of CXR for detecting active TB [8–11], computed tomography (CT) has higher image resolution and sensitivity than CXR and can be used to discriminate between active and latent TB, as a complementary or alternative TB screening modality [12–14].
CT should show a better diagnostic yield for active TB compared to CXR, in cases where TB infection was initially revealed during TB screening. However, there are limited data directly comparing the effectiveness of CT and CXR for detecting or excluding active TB in mass screening for LTBI, whereas existing studies target TB investigation mainly in an outbreak situation or healthcare worker population [4,13]. Therefore, we aimed to investigate the effectiveness and safety of CT as an initial diagnostic modality to exclude active TB, in mass screening for LTBI of the general population of a country with an intermediate TB burden.
METHODS
Study population
This study was conducted from January 2015 to March 2018 at the Seoul Metropolitan Government Seoul National University Boramae Medical Center, a tertiary referral hospital in South Korea. In South Korea, as part of the National TB Elimination Project, mass screening for LTBI (tuberculosis epidemiological investigation on congregated settings) has been underway for workers in collective facilities since 2017. According to an interim report for 3 months from May to August 2017 from the Korea Centers for Disease Control and Prevention, 21.8% of 298,675 test subjects were confirmed as TB-infected patients [6]. They were referred to hospitals for the exclusion of active TB and treatment of LTBI. For TB-infected patients, imaging tests including chest CT were covered by the National Health Insurance in Korea without patient payment. In the Korean medical system, the waiting time required to perform CT was also short, within 1 week, and non-contrast chest CT is enough to exclude active TB without risk of exposure to radiocontrast dye. In this background, CT scans for TB-infected patients could be performed frequently. As clinical experiences of active TB patients not detected by CXR but diagnosed with chest CT were accumulated, chest CT was performed relatively often as an initial examination in our center. We retrospectively reviewed the electronic medical records of patients who were confirmed as TB infection during mandatory mass screening, and who visited our center for additional evaluation. We included patients who were aged > 20 years and underwent a radiological examination to exclude active TB. We excluded patients evaluated after exposure to an active TB patient. We also excluded patients who had a history of treatment for active TB or LTBI, or were diagnosed with extrapulmonary TB, due to the difficulty of interpreting positive LTBI test results and the limitations associated with diagnosis based on CXR, respectively. This study was approved by the Institutional Review Board of the Seoul Metropolitan Government Seoul National University Boramae Medical Center (IRB no. 30-2018-6), and waived the requirement for informed patient consent due to the retrospective nature of the study.
Group definitions
The subjects were assigned to the CXR or chest CT group according to on whether CXR or chest CT was used as the initial diagnostic test at the time of the visit. Patients who underwent CT after normal CXR finding were also assigned to the CT group, because CXR findings alone could not exclude active pulmonary TB. The CXR and CT results were interpreted by radiologists, and the radiological findings regarding TB infection were classified into the following subcategories: (1) calcified granuloma or lymph node; (2) fibronodular scarring; (3) pleural thickening or calcification; (4) cavitation; (5) consolidation; or (6) centrilobular and tree-in-bud nodules [15]. Calcified granuloma or lymph nodes, fibronodular scarring, and pleural thickening or calcification were considered inactive lesions. If a patient complained of sputum at the time of the visit, sputum acid-fast bacilli (AFB) smear and culture were performed; further invasive procedures could be ordered, including bronchoscopy, to obtain an adequate respiratory specimen. We noted instances where these additional tests were performed, and any safety issues arising during them.
Active TB was diagnosed when the following findings were confirmed in respiratory specimens: (1) positive AFB smears; (2) positive AFB cultures but negative AFB smears; or (3) polymerase chain reaction (PCR) positive for Mycobacterium tuberculosis (MTB) but with negative AFB smear and culture results. Active TB was also diagnosed when clinical and radiological findings were consistent with the disease, despite the absence of microbiological evidence for MTB. LTBI was diagnosed when the results of TST or IGRA were positive, and with no clinical and radiological evidence of active TB.
Study outcomes
The primary outcome was the detection rate of active TB according to the radiological modality used initially for diagnosis and to exclude active pulmonary TB. Secondary outcomes were the implementation rate of invasive tests or respiratory specimen tests to rule out active TB, complications of further diagnostic tests, and hospital visits during follow-up.
Statistical analysis
Categorical data are presented as numbers and percentages. Continuous variables are expressed as mean ± standard deviation. Primary and secondary outcomes were analyzed with the chi-square or Fisher’s exact test. A logistic regression model was used to evaluate the risk factors for active TB, including the covariates of age, sex, body mass index, comorbidities, and symptoms. Some of the subjects included in the mass screening had a moderate-to-high risk of active TB, such as human immunodeficiency virus patients, transplantation recipients, those taking tumor necrosis factor (TNF) blockers, and those receiving the steroid maintenance therapy. Additional sensitivity analyses were performed excluding these patients, to evaluate the outcomes in a sample more representative of the general population. Odd ratios (ORs) and adjusted ORs (aORs) were calculated with 95% confidence intervals (CIs). Number needed to screen is defined as the number of subjects who need to be screened for the study period to prevent one adverse event (missing active TB) [16,17]. All A p value < 0.05 was considered significant. All analyses were conducted using R studio (R Foundation for Statistical Computing, Vienna, Austria) and SPSS software version 21.0 (IBM Corp., Armonk, NY, USA).
RESULTS
Baseline characteristics
A total of 822 patients were screened at the Seoul Metropolitan Government Seoul National University Boramae Medical Center between January 2015 and March 2018 (Fig. 1). In total, 542 patients who had a TB infection detected by mass screening, and who underwent a further radiological evaluation, were included in the final analyses. Of these 542 patients, 315 and 227 underwent CXR and chest CT, respectively, as initial radiological studies to exclude active TB. Among the patients with CXR results, 93 underwent CT after normal CXR. Ultimately, 222 and 320 patients were assigned to the CXR and CT groups, respectively.
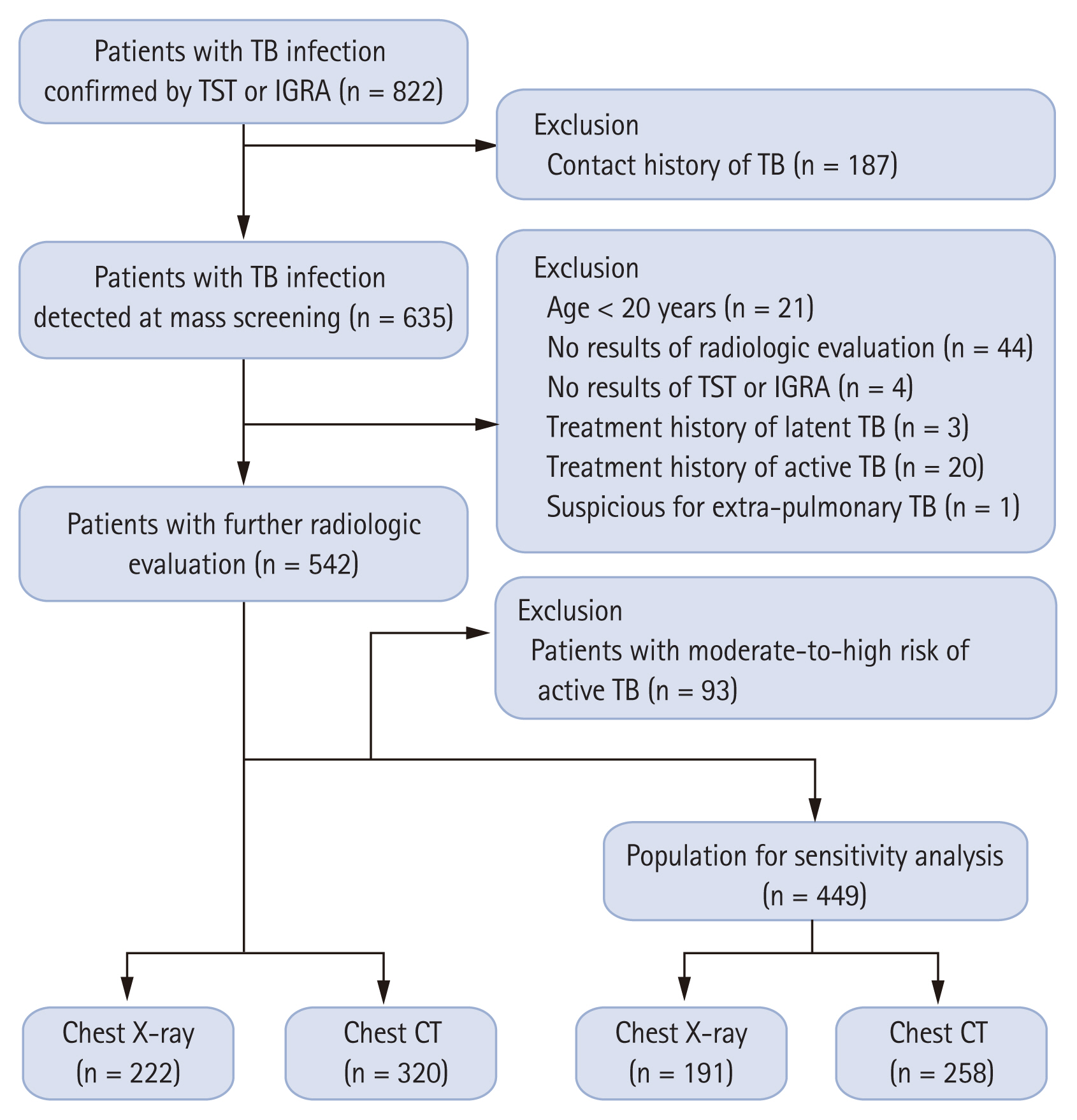
Flow diagram of the study. TB, tuberculosis; TST, tuberculin skin test; IGRA, interferon gamma release assay; CT, computed tomography.
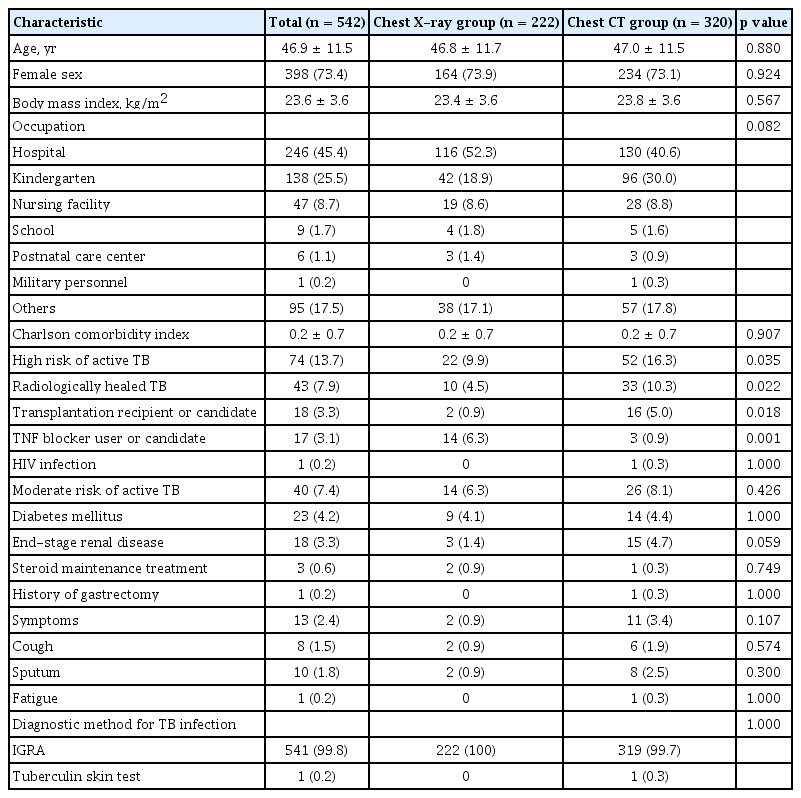
Table 1 lists the baseline demographic and clinical characteristics of the study population. The mean age of the subjects was 46.9 years, and 73.4% were female. The most common occupation was hospital worker (45.4%), and the second most common was kindergarten teacher. Most of the subjects had only a few comorbidities (mean Charlson comorbidity index score, 0.2), and considering the comorbidities, 13.7% and 7.4% of the patients in whom TB infection was confirmed were at high and moderate risk of developing active TB in the future, respectively. Among the comorbidities classified as high risk factors for TB, radiologically healed TB lesions (7.9%) and diabetes mellitus (4.2%) were the most common. No subject had silicosis, head and neck cancer, or a hematological malignancy. Only 2.4% of the subjects had symptoms at the time of the visit. Almost all subjects (99.8%) were diagnosed with TB infection by IGRA.
The baseline characteristics of the study population were not different between the CXR and chest CT groups, except in terms of the proportion of subjects at high risk of active TB. The CXR group had more TNF blocker users or candidates (6.3% vs. 0.9%, p = 0.001), and the chest CT group had more radiologically healed TB findings (10.3% vs. 4.5%, p = 0.022) and transplantation recipients or candidates (5.0% vs. 0.9%, p = 0.018).
Diagnostic process for detecting TB and related events
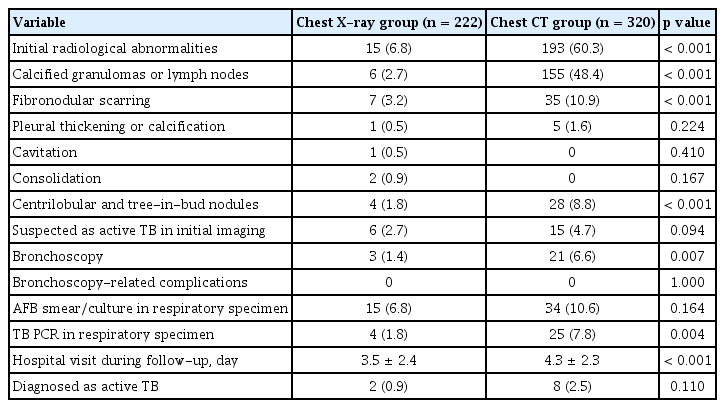
The detection rate for active TB tended to be higher in the CT group than in the CXR group, (2.5% vs. 0.9%, p = 0.110) (Table 2). Radiological abnormalities were significantly more frequent on initial images in the CT group (60.3% vs. 6.8%, p < 0.001). In the CT group, inactive lesions (calcified granuloma or lymph nodes, fibronodular scarring) were found more frequently, although more active lesions (centrilobular and tree-in-bud nodules) were also found. However, no group difference was observed in the number of lesions suspected by the clinician of being active TB.
During the subsequent process to diagnose active TB, the application rate of bronchoscopy, a representative invasive procedure, was higher in the CT group than in the CXR group (6.6% vs. 1.4%, p = 0.007). No bronchoscopy-related complications were reported. The application rates of AFB smear/culture and TB PCR using a respiratory specimen were also higher in the CT group, although a statistical difference was only observed for the TB PCR test. The frequency of hospital visits during follow-up was also significantly higher in the CT group than in the CXR group (4.3 ± 2.3 vs. 3.5 ± 2.4, p < 0.001).
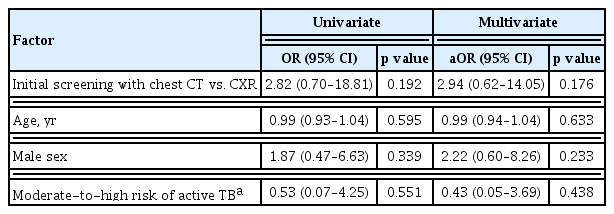
In the overall study population, 10 patients (1.92%) were finally diagnosed with active pulmonary TB, and the others were diagnosed with LTBI. The baseline characteristics were not different between the active TB and LTBI groups, except for the radiological findings (Supplementary Table 1). The LTBI group had more calcified granuloma or lymph node lesions, which are typical inactive radiologic findings, whereas the active TB group had more consolidation and centrilobular/tree-in-bud nodules, suggesting active inflammatory lesions. However, initial screening with chest CT instead of CXR was not associated with a higher rate of detection of active TB in the univariate analysis, even after adjusting for age, sex, and the comorbidity of moderate-to-high risk of active TB (aOR, 2.94; 95% CI, 0.62 to 14.05; p = 0.176) (Table 3). The number of subjects needed to screen with chest CT was 62, which means that 62 chest CTs should have been performed instead of one CXR to avoid missing one patient with active TB.
Radiological findings of active TB
Table 4 lists the clinical characteristics of the 10 patients diagnosed with active TB. None of the patients reported any respiratory symptoms, and only one patient had a comorbid disease (end-stage renal disease). All patients had abnormal findings on the CT scan, but only two had abnormal findings on CXR, despite the obvious abnormalities on the CT.
Sensitivity analysis
A sensitivity analysis was carried out excluding subjects with moderate-to-high risk factors for active TB, to better reflect the general population. No significant differences in baseline characteristics were observed between the CXR and chest CT groups in the sensitivity analysis (Supplementary Table 2). Similar to the results of the primary analysis, the detection rate of active TB tended to be higher in the CT group than in the CXR group (3.1% vs. 0.5%, p = 0.085) (Supplementary Table 3). The number of subjects needed to screen with chest CT, instead of CXR, to exclude a patient with TB was 38. Radiological abnormalities were found more frequently in the chest CT group, and bronchoscopy and the TB PCR test were performed more often in that group. Hospital visits were significantly more frequent in the chest CT group than the CXR group. Initial screening with chest CT was not associated with a higher rate of detection of active TB in the sensitivity analysis population (Supplementary Table 4). The results of the sensitivity analysis were consistent with those of the primary analysis.
DISCUSSION
We hypothesized that chest CT would be more effective than CXR as an initial screening method to exclude active TB, and differentiate between active TB and LTBI in patients with a TB infection detected by mass screening in a country with an intermediate TB burden. However, although chest CT detected more radiological abnormalities in subjects with TB infection, no difference was observed in the rate of detection of patients with active TB between the imaging modalities. Chest CT was associated with additional invasive TB tests using bronchoscopy and respiratory specimens, and a significantly higher frequency of hospital visits.
Although CXR showed good sensitivity (and poor specificity) to diagnose pulmonary TB, some studies have shown that use of CXR in active TB screening programs results in a low diagnostic yield due to limited sensitivity, and also increase the risk of reactivation [10,11]. Chest CT detects more radiological abnormalities than CXR, as confirmed in this study, and can be used to distinguish between active and inactive lesions (because CT is able to reveal the nature of a lesion in more detail) [18]. Chest CT may be useful as a complementary imaging modality to CXR during the screening procedure, particularly in patients with healed TB lesions, or in specific groups of patients at risk of TB reactivation. Previous studies of TB contact investigations reported that chest CT diagnoses active TB better than CXR in subgroups at high risk of infection [12,13].
Some studies have suggested that CT may be a more sensitive screening tool than CXR for other diseases besides TB. For example, the National Lung Screening Trial showed that screening with low-dose CT in a high risk lung cancer group reduced mortality from lung cancer compared to CXR [19]. Another study reported that chest CT improved the diagnostic accuracy for pneumonia, thus reducing the rate of unnecessary antibiotic therapy in elderly patients suspected to have the disease [20].
However, the possibility that chest CT is a more sensitive tool to diagnose TB than CXR does not necessarily mean that CT is appropriate for a mass screening program. In terms of lung cancer screening, there is an overdiagnosis issue associated with CT. Chest CT can be used initially to locate many suspicious lesions, and lead to early diagnosis of lung cancer, which may not actually cause a difference in the subsequent clinical course [21,22]. In this study, radiological abnormalities on initial imaging were 8.87 times more frequent in the chest CT group than in the CXR group, but there was no significant difference in the proportion of suspected and confirmed TB cases between the two groups. CT may detect lesions that mimic TB due to its high sensitivity; however, the clinical significance of those radiologic findings is unclear in the absence of microbiological evidence [23]. Transient inflammatory lesions that resolve spontaneously may also be detected, as well as lesions with other differential diagnoses having centrilobular or tree-in-bud nodules [24–26]. If a screening test has high sensitivity with low specificity, many false-positive results can lead to additional, unnecessary examinations being ordered, consistent with the results of this study.
The risk-benefit and cost-effectiveness ratios must be considered to determine the most appropriate method for mass screening. The effectiveness of TB detection should be weighed against the higher radiation hazard of CT, increased medical costs due to additional testing, and risk of complications following invasive tests before recommending CT as a screening tool for the general population [13,27]. Given the nature of mass screening, the risks posed by a given screening test will affect many people. Therefore, the clinical relevance of mass TB screening should be determined considering regional epidemiology and healthcare system characteristics [28]. The results of this study for mass screening population in a country of intermediate TB burden confirmed that CT conferred no additional benefit over CXR, but significantly increased patient risk and costs; thus, it was not superior to CXR as a screening test for active TB in patients with a TB infection, even after excluding subjects with moderate-to-high risk of developing active TB from the analysis. The use of CT as an initial diagnostic test for mass screening of a TB-infected population was not supported by this study.
This study had several limitations. First, the level of evidence was limited by the retrospective design. Second, this study included a TB-infected population rather than a general population without a confirmed TB infection. In addition, the results of this study were confirmed in the mass screening population, which is different from other previous studies, such as study for contact investigation in outbreak situation. So, it is limited to apply our results to the area of LTBI diagnosis in general population. Third, regional characteristics should be considered when evaluating a screening program. As this study was conducted in a single country with an intermediate TB burden, the results cannot be generalized to other countries without due consideration of the TB epidemiology therein. Fourth, we did not perform a cost-effectiveness analysis for all of the modalities. Further research is needed to assess TB in more large and various population whether chest CT in the mass screening for TB-infected patients will be beneficial to diagnosis active TB, considering its high sensitivity.
In conclusion, detection rates of active TB were not different between chest CT and CXR (as the initial diagnostic method), in a mass screening program in an intermediate-burden country. However, implementing CT significantly increased the likelihood of further invasive procedures, respiratory specimen tests, and hospital visits.
KEY MESSAGE
1. Chest computed tomography (CT) detected more radiological abnormalities in subjects with tuberculosis (TB) infection detected by mass screening; however, did not improve the detection rate of active TB compared to chest X-ray.
2. The use of chest CT as initial diagnostic method for TB infection was associated with additional invasive TB tests using bronchoscopy and respiratory specimens, and a significantly higher frequency of hospital visits.
Notes
No potential conflict of interest relevant to this article was reported.