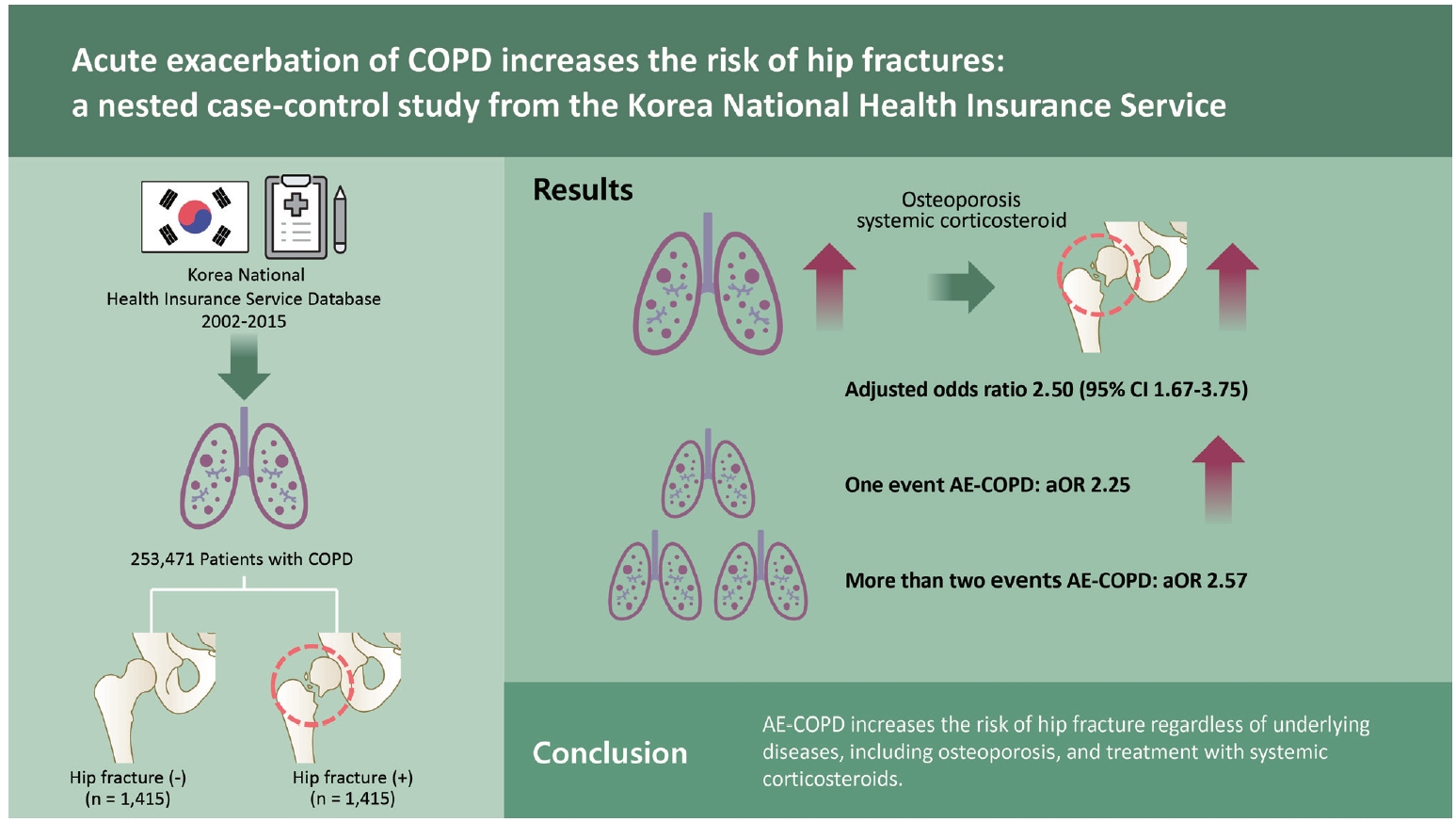
Acute exacerbation of COPD increases the risk of hip fractures: a nested case-control study from the Korea National Health Insurance Service
Article information
Abstract
Background/Aims
Hip fracture and acute exacerbation of chronic obstructive pulmonary disease (AE-COPD) could increase mortality in patients with COPD. There are no data on the relationship between AE-COPD and hip fracture, which may significantly affect the prognosis of patients with COPD. Therefore, we conducted this study to determine the effects of AE-COPD on hip fractures in patients with COPD.
Methods
This retrospective, nested, case-control study included 253,471 patients with COPD (≥ 40 years of age) identified from the Korea National Health Insurance Service-National Health Screening Cohort (NHIS-HEALS) from 2002 to 2015. Among 176,598 patients with COPD, 1,415 patients with hip fractures were identified. Each case was matched to one control for age (within 10 years), sex, and year of COPD diagnosis. We estimated the adjusted odds ratios (aORs) and 95% confidence intervals (CIs) for hip fractures associated with AE-COPD using conditional logistic regression analysis, adjusting for underlying diseases and smoking history.
Results
In patients with AE-COPD, the risk of hip fracture was 2.50 times higher, regardless of systemic corticosteroid use and underlying disease (aOR, 2.50; 95% CI, 1.67 to 3.75). The risk of hip fracture increased if there was one episode of AE in the year before hip fractures (aOR, 2.25; 95% CI, 1.66 to 3.05). Moreover, the risk of hip fracture also increased in patients with more than two episodes of AE the year before hip fractures (aOR, 2.57; 95% CI, 1.61 to 4.10).
Conclusions
AE-COPD increases the risk of hip fracture regardless of underlying diseases, including osteoporosis, and treatment with systemic corticosteroids.
INTRODUCTION
Chronic obstructive pulmonary disease (COPD) is a heterogeneous disease characterized by chronic airway inflammation and airflow limitation and is one of the leading causes of death worldwide [1,2]. Patients with COPD have a higher risk of death following fractures than those without COPD, regardless of the site of fracture [3].
Hip fractures can cause serious deterioration of physical function, decrease the quality of life, and increase mortality in elderly patients despite appropriate surgical treatment [4,5]. According to a recent population-based study, COPD could increase the risk of hip fracture by 1.57 times [6]. In particular, in patients with COPD with hip fractures, the 1-year mortality is 3 to 5 times higher than that in patients without hip fractures [7]. Therefore, efforts have been made to identify the risk factors for hip fractures in patients with COPD. In patients with COPD, osteoporosis is a major comorbidity that can increase the incidence of fractures and further reduce lung function and quality of life [8–10].
Acute exacerbation of COPD (AE-COPD) is an important condition that can increase the mortality in patients with COPD and lead to deterioration of comorbidities. To the best of our knowledge, there are no data on the relationship between AE-COPD and hip fractures, which could significantly affect the prognosis of patients with COPD. Therefore, we conducted this study to determine the effects of AE-COPD on hip fracture in patients with COPD.
METHODS
Data source
Our study is based on data from the National Health Insurance Service-National Health Screening Cohort (NHIS-HEALS) in South Korea [11]. Since 1995, the NHIS has provided a general national health screening program to improve the health of Koreans through disease prevention and early detection [12]. All diagnoses were coded using the International Classification of Diseases (ICD) and Related Health Problems system, with high precision for diagnoses, particularly for fractures.
Study design
This was a retrospective, nested, and case-control study. The case group was defined as patients with COPD diagnosed with a hip fracture between 2004 and 2015, and the control group was defined as patients with COPD who had never been diagnosed with a hip fracture during the study period. Both the case and control groups only included patients over 40 years of age. For each case, a control was matched for age (within 10 years), sex, and year of COPD diagnosis.
COPD patients were defined as those with COPD diagnostic codes (J42–J44, except J430) and treatment with COPD medications including the following: (1) inhaled long-acting muscarinic antagonists; (2) inhaled long-acting beta-2 agonists (LABA); (3) inhaled corticosteroids (ICS); (4) ICS plus LABA; (5) inhaled short-acting muscarinic antagonists; (6) inhaled short-acting beta-2 agonists; (7) methylxanthines; (8) oral corticosteroids; and/or (9) systemic beta-2 agonists. In the COPD cohort, patients with a hip fracture diagnostic code (S72) were defined as hip fracture patients. Patients with AE-COPD were defined as those who were prescribed inhalation therapy and systemic steroids, with records of hospitalization and emergency room (ER) visits based on the health insurance claims code. In addition, the cumulative steroid usage days within 1 year before hip fracture were divided into low and high with 90 days as the cut-off, based on the American College of Rheumatology guideline that osteoporosis is more likely with 90 days of systemic steroid use [13,14]. The study protocol was approved by the Chung-Ang University Hospital Institutional Review Board (1811-015-16223), and the requirement for written informed consent was waived.
Variables
Each matched group was stratified into 15-year age intervals as follows: 40–54, 55–64, and ≥ 65 years. Age was defined as the age at the time of COPD diagnosis. We classified patients according to their year of COPD diagnosis according to the following 5-year intervals: 2002–2006, 2007–2011, and 2012–2015. The medical histories of the patients were evaluated using ICD-10 codes and the Korea Health Insurance Review & Assessment Service (HIRA) codes. Diagnostic accuracy was determined based on the diagnosis of ischemic heart disease (I24 and I25), congestive heart failure (I50), hypertension (I101 and I109), osteoporosis (M80-M82), depressive disorder (F32.9, F33), arthritis (M15), diabetes mellitus (E10, E11, and E14), anemia (D50-D53, D64), and low back pain (M5450, M5455-M5459). In addition, smoking history was divided into four categories: missing, never smoker, ex-smoker, and current smoker.
Statistical analysis
Categorical variables were expressed as numbers and percentages, and continuous variables were expressed as medians and standard deviations. Individual groups were compared using the chi-squared test and Student’s t test. A multivariable conditional logistic regression model was used to compute the odds ratios and 95% confidence intervals (CIs). Potential confounders included adjusted smoking history and underlying disease, which were identified by comparing the features of the two groups (Table 1). The effect estimates were adjusted for covariates that were significantly associated with mortality (p < 0.1). In the multivariable model, missing values were included as dummy variables. The precision of the effect estimates is reported using 95% CIs. Statistical analyses were conducted using SAS Enterprise Guide version 7.1 (SAS Institute Inc., Cary, NC, USA).
RESULTS
Study population
Among the 253,471 suspected COPD patients, 176,598 were enrolled after the exclusion of 76,873 patients who had not been prescribed related medications. We stratified the 176,598 patients with COPD into two groups according to their hip fracture status, and 1,415 patients were 1:1 matched according to age, sex, and year of COPD diagnosis (Fig. 1).

Flow chart of the study. COPD, chronic obstructive pulmonary disease. aInhaled corticosteroid + long-acting beta-2 agonist (LABA), long-acting muscarinic antagonist (LAMA), LABA, short-acting beta-2 agonist, short-acting muscarinic antagonist, LABA + LAMA, theophylline, phosphodiesterase-4 inhibitor.
Clinical features of patients with COPD with and without hip fractures
We compared the clinical features of patients with COPD with and without hip fractures. Sex, age, and years of COPD diagnosis were matched. Underlying diseases, such as ischemic heart disease, congestive heart failure, hypertension, osteoporosis, depressive disorder, arthritis, diabetes mellitus, anemia, and low back pain, were more frequent in the hip fracture group. The number of intensive care unit admissions and ER visits was significantly higher in the COPD group (Table 1).
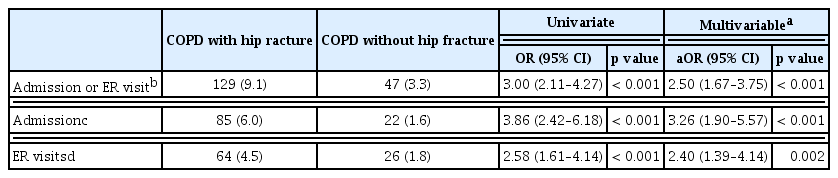
Effects of AE-COPD and systemic steroid use on hip fractures
We evaluated the effect of AE-COPD and systemic corticosteroids on hip fractures in patients with COPD (Table 2). Patients were stratified into four groups according to the AE-COPD and systemic corticosteroid use, and each group was compared based on a group with no AE-COPD and low systemic corticosteroid use. Hip fractures were significantly increased in patients with high systemic corticosteroid use (adjusted odds ratio [aOR], 2.94; 95% CI, 1.81 to 4.78). In patients with AE-COPD, hip fractures significantly increased regardless of systemic corticosteroid use (aOR, 2.25; 95% CI, 1.45 to 3.48).
Effects of AE-COPD on hip fractures
We also evaluated the effect of AE-COPD on hip fractures in patients with COPD (Table 3). In patients with AE-COPD, the risk of hip fractures was 2.50 times higher, regardless of systemic corticosteroid use and underlying diseases (aOR, 2.50; 95% CI, 1.67 to 3.75). In admitted patients, hip fractures were significantly more likely, regardless of underlying diseases and systemic corticosteroid use (aOR, 3.26; 95% CI, 1.90 to 5.57). In patients with an ER visit only, hip fractures were significantly more likely, regardless of underlying diseases and systemic corticosteroid use (aOR, 2.40; 95% CI, 1.39 to 4.14).
Impact of AE-COPD frequency on patients with hip fractures
We evaluated the risk of hip fractures according to annual AE-COPD in the 1 year before the occurrence of hip fractures (Fig. 2). First, if there was one AE-COPD before the hip fracture, the risk of a hip fracture increased by approximately 2.25 times (aOR, 2.25; 95% CI, 1.66 to 3.05), and if there were more than two AE-COPD events in the year before the hip fracture, the risk of a hip fracture increased by approximately 2.57 times (aOR, 2.57; 95% CI, 1.61 to 4.10). Second, based on the total number of annual AE-COPD events from COPD diagnosis to a hip fracture, if there was one AE-COPD, the risk of a hip fracture increased by approximately 1.67 times (aOR, 1.67; 95% CI, 1.06 to 2.62). In addition, if there were more than two AE-COPD events, the risk of a hip fracture increased by approximately 2.01 times (aOR, 2.01; 95% CI, 1.02 to 3.95) based on the total number of annual AE-COPD events between COPD diagnosis and a hip fracture.

Multivariable conditional logistic regression according to the number of acute exacerbations per year. CI, confidence interval; COPD, chronic obstructive pulmonary disease; HR, hazard ratio. aAdjusted for steroid use, smoking history, ischemic heart disease, congestive heart failure, hypertension, osteoporosis, depressive disorder, arthritis, diabetes mellitus, anemia, lower back pain, bThe number of acute exacerbation per year that occurred 1 year before the event of hip fracture, cThe number of acute exacerbation per year that times of COPD diagnosis to the time of the hip fracture.
DISCUSSION
In this population-based, nested case-control study, we identified that AE-COPD was associated with an increased risk of hip fractures in patients with COPD. In particular, the risk of hip fractures was significantly higher when AE-COPD occurred more frequently during the 1 year before a hip fracture. In addition, the risk of a hip fracture was significantly higher when the annual frequency of AE-COPD before a hip fracture was higher. These results are meaningful because they are established after adjusting for factors such as steroid use and underlying disease (including osteoporosis), which are known to increase the risk of hip fractures.
AE-COPD is a heterogeneous event in COPD, and it is difficult to predict its course [15,16]. AE-COPD is associated with reduced quality of life [17], worsening lung function [18], and increased mortality [19,20]. Previous studies have focused on the use of systemic corticosteroids and their relationship with osteoporosis [21–23]. In patients with COPD, osteoporosis is one of the most common comorbidities that increases the risk of hip fractures [24], and treatment of AE-COPD with systemic steroids could also increase the risk of hip fractures [25]. In our study, in patients with COPD, using systemic corticosteroids for more than 90 days was associated with increasing hip fracture risk even after adjusting for comorbidities. Therefore, if patients with COPD have frequent AE events, bone protective management and monitoring osteoporosis using bone mineral density testing should be considered to reduce the risk of hip fractures. In the treatment of AE-COPD, continued efforts to reduce the duration of systemic steroid administration are also important in reducing the risk of hip fractures.
Our study had several strengths. First, to the best of our knowledge, this is the first population-based cohort study to compare the risk of hip fractures and AE-COPD. Second, this was a nationwide cohort study based on the analysis of a large representative population from a validated database. The data are large-scale, extensive, and stable because they are constructed based on nationwide health insurance data generated by the government or by public institution involvement.
Despite its strengths, our study has several potential limitations. First, there are limitations in the operational definition of AE-COPD based on health insurance claim codes. We could not exclude cases in which steroids were prescribed for reasons other than AE-COPD at the time of ER visit for hospitalization. Second, we did not have information that could evaluate the severity of COPD (such as spirometry, the modified Medical Research Council scale [mMRC], or COPD assessment test [CAT]) and risk of hip fractures (such as bone mineral density, diet, or weight at the time of occurrence of a hip fracture). Therefore, further studies based on lung function or bone mineral density are required to increase reliability. Third, even though the control group was matched by age, sex, and year of COPD diagnosis, there were significant differences in the underlying diseases between the case and control groups. Fourth, in this study, steroid administration history was analyzed only based on the cumulative period of systemic steroid use. The amount of systemic corticosteroids that the patients actually used could not be accurately determined due to limitations of the NHIS-HEALS database.
In conclusion, AE-COPD might increase the risk of hip fractures regardless of underlying diseases, including osteoporosis, and systemic corticosteroid use.
KEY MESSAGE
1. Acute exacerbation of chronic obstructive pulmonary disease (AE-COPD) is associated with an increased risk of hip fractures, regardless of underlying diseases, including osteoporosis.
2. AE-COPD is associated with an increased risk of hip fractures, regardless of the use of systemic corticosteroids.
Notes
No potential conflict of interest relevant to this article was reported.
Acknowledgements
This study was supported by grants from the Alumni Association of Division of Pulmonary, Allergy and Critical Care Medicine, Internal Medicine of Chung-Ang University Hospital (Ungye Research Funds). The funders had no role in the study design, data collection and analysis, decision to publish, or preparation of the manuscript.