Diabetic cystopathy preceding renal microabscess with papillary necrosis
Article information
A 31-year-old woman without any prior disease presented to the emergency department complaining of progressive distention of the abdomen for 10 days. Her medical history was unremarkable, and she was not on any medication. The patient stated she had difficulty urinating for the past 7 days. Physical examination revealed a large palpable mass in the abdomen. Laboratory studies revealed the following: serum glucose 807 mg/dL, glycated hemoglobin 14.7% without evidence of ketoacidosis, blood urea nitrogen 104.3 mg/dL, creatinine 8.47 mg/dL, corrected sodium 128 mEq/L, potassium 4.8 mEq/L, urine creatinine 23.8 mg/dL, and urine sodium 38 mEq/L. Her fasting and postprandial C-peptide levels were 1.27 and 3.58 ng/mL, respectively, suggestive of first diagnosed type 2 diabetes. The calculated fractional excretion of sodium was 10.1%, highly suggestive of post-renal acute renal failure. Abdomen and pelvis computed tomography revealed a marked distended bladder (Fig. 1A) with bilateral hydronephrosis and hydroureters (Fig. 1B). A Foley catheter was inserted initially presenting 3,500 mL of urine. Three days after Foley insertion, the serum creatinine level fell under 1.0 mg/dL. However, the patient failed to remove the Foley catheter despite the use of anticholinergics. One month later, renal microabscess with papillary necrosis developed in both kidneys (Fig. 2). Even with intensive antibiotics and glucose management, the patient experienced kidney failure and thus hemodialysis treatment was initiated.

Computerized tomography of the abdomen and pelvis revealing (A) massive distention of the urinary bladder (red arrow), sagittal view; (B) hydronephrosis and hydroureter, transverse view.
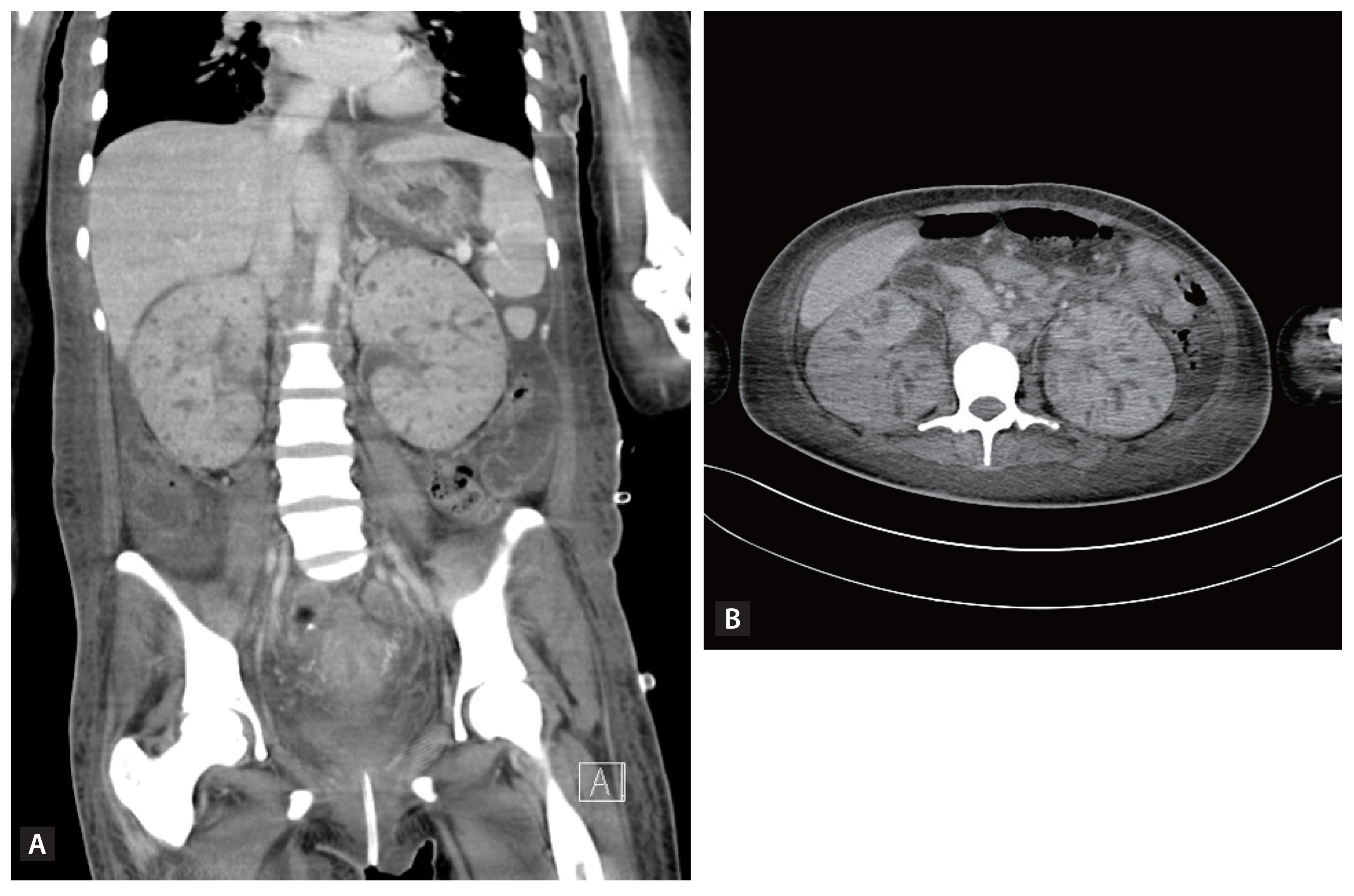
Computerized tomography of the abdomen and pelvis, revealing diffuse enlargement of both kidneys with decreased enhancement. Multifocal small hypodense lesions in both kidneys suggest microabscess and papillary necrosis. (A) Coronal view, (B) transverse view.
Impaired voiding is one of the most common sequelae of diabetic cystopathy. Damage to the innervation of the visceral fibers in the lower urinary tract can result in both post voiding residual volume and bladder retention, as well as kidney infections, including pyelonephritis and renal abscess. This case highlights the poor prognosis of diabetic cystopathy resulting in hemodialysis. In patients presenting with abdominal distention accompanied by hyperglycemia, it is crucial to consider a differential diagnosis of diabetic cystopathy and start intensive primary management to prevent renal loss.
Notes
No potential conflict of interest relevant to this article was reported.
