Boerhaave syndrome initially presenting as acute coronary syndrome with systolic total obstruction of myocardial bridge
Article information
Chest pain, one of common and important complaints, encompasses many differential diagnoses including both cardiac and non-cardiac disorders. Among them, non-cardiac disorders sometimes imitate life-threatening cardiac disorders. We present a case of Boerhaave syndrome (BS) mimicking ST-segment elevation acute coronary syndrome (ACS) with systolic total obstruction of myocardial bridge (MB).
A 50-year-old man presented with squeezing chest pain just after binge drinking in the evening. On the electrocardiogram, ST-segment was elevated at lead II and III (Supplementary Fig. 1). Because we initially suspected ST-segment elevation ACS, emergent coronary angiogram was promptly performed. It showed very severe systolic milking at left anterior descending coronary artery to total obstruction, indicating severe MB (Fig. 1A, Supplementary Videos 1 and 2). However, there was no any other fixed obstruction in all coronary arteries (Supplementary Videos 3). Thus, we performed additional diagnostic modalities, including contrast-enhanced chest computed tomography angiography and pharyngoesophagogram, showing large pneumomediastinum with esophago-pleuro-pulmonary fistula (Fig. 1B and 1C, Supplementary Videos 4 and 5), suggesting BS. Therefore, urgent operation was done including posterolateral thoracotomy, dissection of mediastinal pleura, primary repair of esophagus and massive irrigation (Fig. 1D). Postoperative pharyngoesophagogram showed no remarkable mucosal destruction or passage disturbance in esophagus and pharynx (Supplementary Video 6). After surgery and postoperative care, chest pain was diminished then the patient was discharged successfully.
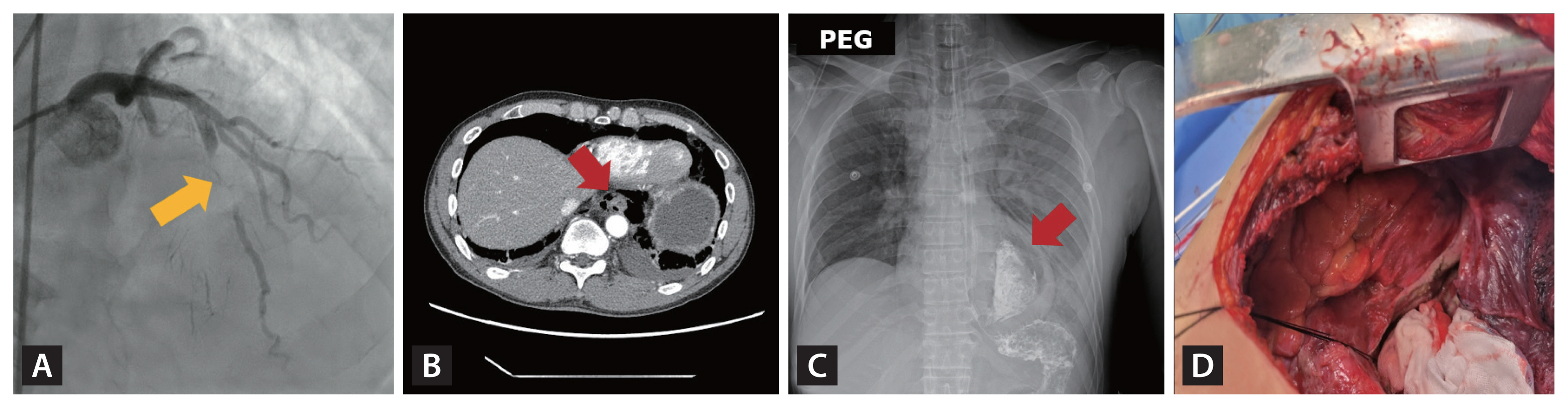
Because the patient was initially suspected of acute coronary syndrome, coronary angiogram was urgently performed. (A) Left-selective coronary angiogram shows full coronary obstruction (yellow arrow) with severe systolic milking in middle portion of left anterior descending coronary artery. (B, C) Contrast-enhanced chest computed tomography and pharyngoesophagogram (PEG) showed large pneumomediastinum (red arrow) with esophago-pleuro-pulmonary fistula (red arrow). (D) Therefore, urgent operation was done including posterolateral thoracotomy, dissection of mediastinal pleura, primary repair of esophagus and massive irrigation.
BS is a very rare condition generally occurring owing to the increase in the intraesophageal pressure. It is the first case of BS with systolic total obstruction of MB, initially presenting as ACS, but was surgically treated with improvement of chest pain. Clinicians need to pay more attention then not to forget that BS, a lethal gastrointestinal tract disorder, is also one of differential diagnoses of chest pain. The present study was approved by the Institutional Review Board at Chonnam National University Hospital (Approval No. CNUH-EXP-2022-266). Informed consent was obtained from the patient.
Supplementary Information
Left-selective angiogram showed very severe systolic milking at left anterior descending coronary artery to total obstruction, suggesting severe myocardial bridge.
Left-selective angiogram showed very severe systolic milking at left anterior descending coronary artery to total obstruction, suggesting severe myocardial bridge.
Contrast-enhanced chest computed tomography demonstrated large pneumomediastinum with esophago-pleuro-pulmonary fistula.
Acknowledgments
This case was selected as one of the excellent abstract presentations of the 73rd Fall Conference of the Korean Association of Internal Medicine in 2022.
Notes
No potential conflict of interest relevant to this article was reported.
