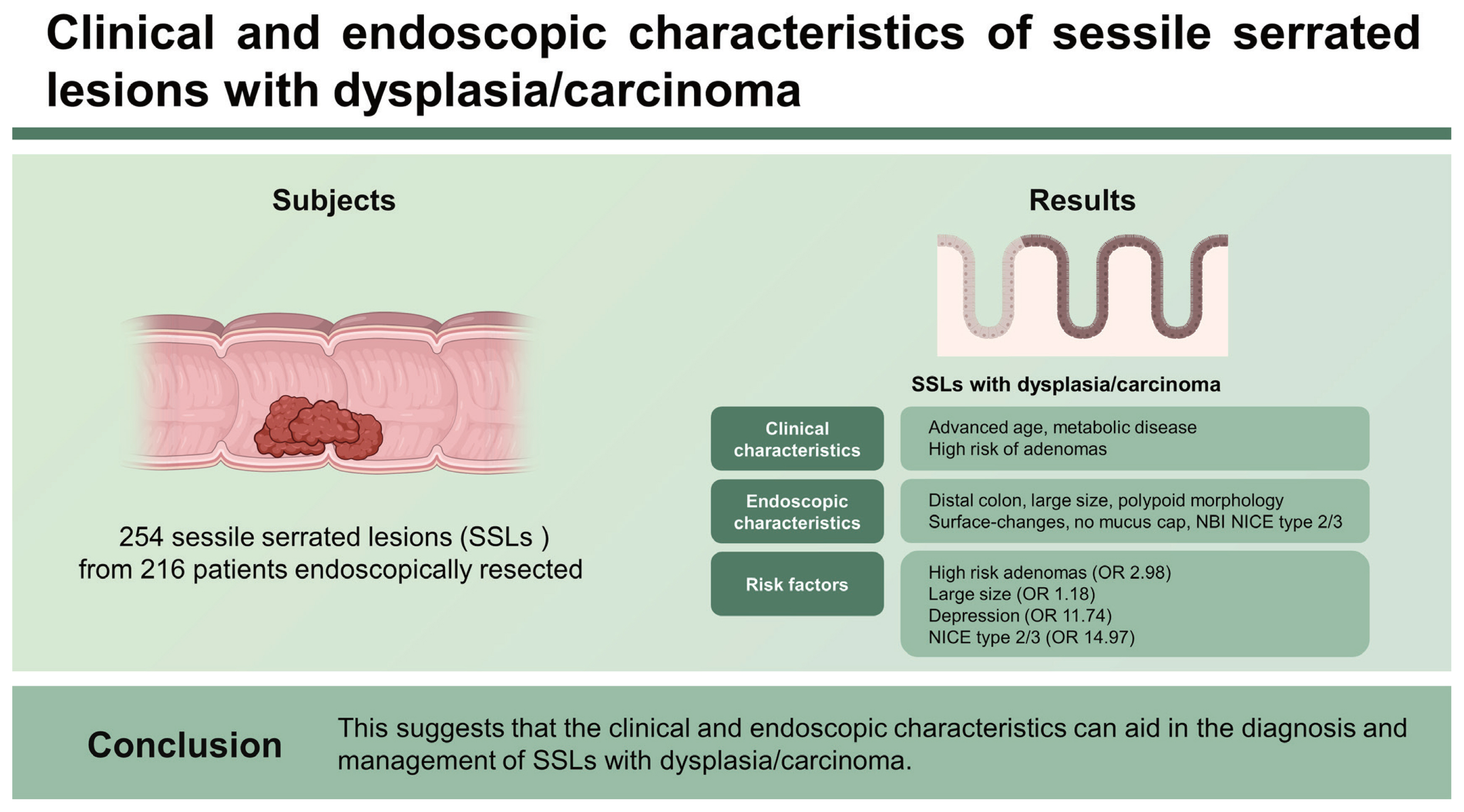
Clinical and endoscopic characteristics of sessile serrated lesions with dysplasia/carcinoma
Article information
Abstract
Background/Aims
Some sessile serrated lesions (SSLs) progress into dysplasia and colorectal cancer, however, the clinical and endoscopic characteristics of SSLs with dysplasia remain to be determined. In this study, we elucidated these characteristics in SSLs with dysplasia/carcinoma, compared with those of SSLs without dysplasia.
Methods
We retrospectively collected the clinical, endoscopic, and pathological data of 254 SSLs from 216 patients endoscopically resected between January 2009 and December 2020.
Results
All SSLs included 179 without dysplasia and 75 with dysplasia/carcinoma, including 55 with low-grade dysplasia, 10 with high-grade dysplasia, and 10 with submucosal cancer. In clinical characteristics, SSLs with dysplasia/carcinoma were significantly associated with advanced age, metabolic diseases, and high-risk adenomas. In endoscopic characteristics, SSLs with dysplasia/carcinoma were significantly associated with the distal colon, large size, polypoid morphology, surface-changes, no mucus cap, and narrow-band imaging international colorectal endoscopic classification (NICE) type 2/3. In the multivariate analysis, high-risk adenomas (odds ratio [OR], 2.98; p = 0.01), large size (OR, 1.18; p < 0.01), depression (OR, 11.74; p = 0.03), and NICE type 2/3 (OR, 14.97; p < 0.01) were significantly associated with SSLs with dysplasia/carcinoma.
Conclusions
SSLs had a higher risk of dysplasia in the distal colon than in the proximal colon. SSLs with large size, depression, and adenomatous surface-patterns, as well as those in patients with high-risk adenomas, increased the risk of dysplasia/carcinoma. This suggests that the clinical and endoscopic characteristics can aid in the diagnosis and management of SSLs with dysplasia/carcinoma.
INTRODUCTION
The terms “sessile serrated polyp” and “sessile serrated adenoma” were first introduced by Torlakovic et al. [1] and are similar to hyperplastic polyp grossly but has histologically unique architectural distortion in basal crypt. Recently, the World Health Organization (WHO) has recommended the use of the term sessile serrated lesion (SSL) instead of other terms, such as sessile serrated adenoma, sessile serrated polyp, or sessile serrated adenoma/polyp [2]. SSLs account for up to 8% of colorectal polyps in a screening population [3–5] and their characteristics include predominant location in the right colon, difficult detection, and incomplete resection [6]. Unlike hyperplastic polyps, SSLs progress to SSLs with dysplasia in approximately 4–8% of cases [7,8] and have a malignant potential, that is, the lesions may develop into colorectal cancer with high microsatellite instability through the serrated neoplasia pathway [9–11]. Based on molecular features, approximately 25% of sporadic colorectal cancers develops along the serrated neoplasia pathway [12]. Although SSLs have a long dwelling time of over 10 to 15 years before the development of cancer [4], some SSLs may have a high potential for rapid progression to invasive carcinoma and eventually develop interval cancers [13–17].
SSLs with dysplasia or invasive carcinoma are often difficult to detect with endoscopy and are easily missed as some SSLs with dysplasia or invasive carcinoma have subtle mucosal features [17]. In particular, incomplete resection, which resects only the dysplastic part of the SSL similar to a conventional adenoma and leaves behind the background serrated tissue, can lead to risk of a rapid progression to interval cancer. Therefore, accurate recognition of the clinical and endoscopic characteristics of SSLs with dysplasia is important to prevent the occurrence of interval cancer by reducing the number of incomplete resections and determining appropriate surveillance intervals. Although SSLs with dysplasia or invasive carcinoma have been suggested to be associated with advanced age, female sex, proximal colon, pedunculated morphology, double elevation, central depression, and a reddish hue, data on the clinical and endoscopic characteristics of SSLs with dysplasia or carcinoma in detail remain limited [18–20]. To address this knowledge gap, we aimed to elucidate the clinical and endoscopic characteristics of SSLs with dysplasia/carcinoma and compare them with those of SSLs without dysplasia.
METHODS
Study design and patients
We retrospectively collected clinical, endoscopic, and pathological data regarding SSLs with and without dysplasia/carcinoma that were endoscopically resected and histologically diagnosed at the Gastroenterology Department of The Pusan National University Yangsan Hospital (PNUYH). Between January 2009 and December 2020, 223 patients (261 polyps) were enrolled in the study. Seven patients had no narrow-band imaging (NBI) or close-up imaging. Finally, 216 patients (254 polyps) were assessed in total (Fig. 1). This study was approved by the Institutional Review Board (IRB) of PNUYH (IRB no. 05-2021-020), and informed consent was not required as this was a retrospective study.
Clinical and pathologic analysis
We evaluated the clinical and endoscopic findings according to the pathological type of all patients and polyps, respectively, and analyzed the differences in the clinical and endoscopic characteristics of patients and polyps between SSLs with and without dysplasia.
Metabolic diseases were defined as follows: hypertension (blood pressure ≥ 140/90 mmHg), type 2 diabetes mellitus (fasting blood sugar > 126 mg/dL), or dyslipidemia (total cholesterol ≥ 240 mg/dL) under specific drug treatment. The proximal colon was defined as being proximal to the splenic flexure (i.e., the cecum, ascending colon, and transverse colon). High-risk adenomas were defined as adenomas with villous histology, high-grade dysplasia (HGD), ≥ 10 mm in size, or ≥ 3 adenomas in number [21].
All resected specimens were fixed in 10% formalin, cut into 2-mm sections, and microscopically examined to evaluate the size, histological type, depth of invasion, and status of margins after resection. According to the updated WHO 2019 criteria, the presence of a single unequivocally distorted crypt is considered diagnostic for SSL [22]. Crypt distortion can be present in different forms, such as horizontal crypts, dilated crypts (basal third of the crypt), and/or crypts that have serrations extending in the crypt base. Serrated lesions that did not meet these criteria were diagnosed as hyperplastic polyps. All hyperplastic polyps and SSLs resected during this study were re-assessed in accordance with the WHO 2019 criteria and revised by two dedicated gastrointestinal pathologists (D.H.S. and J.Y.N.). SSLs with dysplasia/carcinoma were required to show (1) a component of an ordinary SSL at the edge of the lesion comprising at least three crypts, one of which must show SSL-type histology, or (2) an abrupt transition from an ordinary SSL to overt cytologic dysplasia or carcinoma within one tissue fragment [23]. For SSLs with invasive carcinoma, we measured the depth of submucosal involvement according to the clinical guidelines of the Japanese Society for Cancer of the Colon and Rectum [24]. The lateral margin status was categorized according to the Japanese criteria as follows: positive, wherein the lateral margin is positive for tumor cells; or indeterminate, wherein glands at the lateral margin are damaged and cannot be evaluated for the presence of neoplasia [25]. All lesions that underwent piecemeal resection were categorized as having indeterminate lateral margins.
Endoscopic analysis
All endoscopic procedures were performed by endoscopists with extensive experience and two endoscopists (H.W.K. and S.B.P.) with > 10 years of experience between them evaluated the endoscopic images using conventional white-light and NBI. All images were categorized as one opinion after a discussion between both endoscopic evaluators. All endoscopic evaluations and resections were performed using high-definition white-light with NBI scopes (Olympus CF-H260AI/HQ290I; Olympus Medical Systems Corp., Tokyo, Japan) with a transparent hood cap (D-201-14304; Olympus Medical Systems Corp.). Macroscopic type was classified according to the Paris-Japanese classification [26]. The size of the lesions was measured by comparing them with open or closed biopsy forceps or polypectomy snares of known diameters. In the case of a large polyp that could not be measured using the above methods, the size of the polyp was determined based on both endoscopic and histological estimations.
SSLs were suspected and resected in cases with at least two endoscopic findings, such as a clouded surface, indistinctive borders, irregular shape, dark spots inside the crypt, or overlying mucus cap [23,27]. A careful examination with conventional endoscopy was followed by NBI endoscopy without magnification. We evaluated the NBI findings of SSL using the NBI International Colorectal Endoscopic Classification (NICE). A careful search was retrospectively conducted for any demarcated area with an adenomatous surface-patterns on the SSL. If detected, the lesion was described as an SSL with dysplasia, and the features of this area were described in detail.
Among the several endoscopic findings, the five surface- changes on white-light colonoscopic images evaluated by two endoscopists were (1) granular surface, (2) focal nodular elevation, (3) depression, (4) redness, and (5) mucus cap (Fig. 2). The five surface-changes were defined as follows: (1) granular surface: diffuse and fine nodular elevations (Fig. 2A, B); (2) focal nodular elevation: prominent elevation with a clear demarcation (Fig. 2C, D); (3) depression: clearly depressed area in the lesion (Fig. 2E, F); (4) redness: relatively clear red/pink area compared with the adjacent mucosa (Fig. 2G, H); and (5) mucus cap: focal collection of mucus (clear, bile-stained, or debris-stained) on the mucosal surface that can be removed with irrigation (Fig. 2I, J).

Five surface findings of sessile serrated lesions with/without dysplasia/carcinoma. (A, B) Granular surface. (C, D) Focal nodular elevation. (E, F) Depression. (G, H) Redness. (I, J) Mucus cap.
The selection of endoscopic resections such as snare resection with/without injection and endoscopic submucosal dissection (ESD) was determined according to various factors. Endoscopic resection was performed for en bloc resection, whereas intended piecemeal resection was performed in cases of impossible en bloc resection due to technical difficulties during snare resection or ESD. ESD for en bloc was mainly performed for SSLs up to 20 mm.
Statistical analysis
All statistical analyses were conducted using SPSS version 26.0 for Windows (SPSS Inc., Chicago, IL, USA). Continuous data were compared using independent t-tests. Categorical analysis of variables was performed using either the chi-square test, Fisher’s exact test or the Kruskal-Wallis test as appropriate. Factors associated with dysplasia in SSLs were assessed using logistic regression analysis (univariate and multivariate analyses). Statistical significance was set at p < 0.05.
RESULTS
Clinical characteristics of patients with SSLs without dysplasia and with dysplasia/carcinoma
The clinical characteristics of 216 patients with SSL are summarized in Table 1, of which 144 patients with SSL without dysplasia and 72 with dysplasia/carcinoma. Mean age was 56.3 ± 12.6 years in patients with all SSLs, 54.7 ± 12.1 years in patients with SSL without dysplasia, and 59.6 ± 13.1 years in patients with SSL with dysplasia/carcinoma. SSLs with dysplasia/carcinoma were significantly associated with advanced age (p < 0.01). SSLs with dysplasia/carcinoma were more frequently associated with female sex and a history of colorectal cancer than SSLs without dysplasia, but the difference was not statistically significant. Metabolic diseases were present in 35.6% of patients with all SSLs, 29.9% of patients with SSL without dysplasia, and 47.2% of patients with SSL with dysplasia/carcinoma and were significantly associated with SSLs with dysplasia/carcinoma (p = 0.01). There was no difference in the indications for colonoscopy between the two groups. In the type of accompanied polyps, SSLs without dysplasia were significantly associated with multiple SSLs (17.4% vs. 5.6%, p = 0.02), whereas SSLs with dysplasia/carcinoma were significantly associated with high-risk adenomas (16.0% vs 27.8%, p = 0.04).
Endoscopic characteristics of SSLs without dysplasia and with dysplasia/carcinoma
The endoscopic and pathological findings of the SSLs are summarized in Table 2. Most SSLs were located in the proximal colon (200/254; 78.7%) and overall SSLs with dysplasia were more frequent in the proximal colon (52/254 [20.5%] vs. 23/254 [9.1%]), but the risk of dysplasia was significantly higher in the distal colon than in the proximal colon (23/54 [42.6%] vs. 52/200 [26.0%), p = 0.02). With regards to size and morphology, SSLs with dysplasia/carcinoma were significantly larger (20.9 ± 13.3 mm vs. 9.5 ± 5.2 mm, p < 0.01) and more polypoid (40.0% vs. 19.0%, p < 0.01) than SSLs without dysplasia, respectively. In the surface-changes, SSLs with dysplasia/carcinoma were significantly associated with granular surface (33.3% vs. 2.2%, p < 0.01), focal nodular elevation (37.3% vs. 2.8%, p < 0.01), depression (14.7% vs. 0.6%, p < 0.01), and redness (17.3% vs. 6.1%, p = 0.01) than SSLs without dysplasia, respectively. However, the mucus cap was significantly associated with SSLs without dysplasia compared with SSLs with dysplasia/carcinoma (26.8% vs. 12.0%, p = 0.01). In NICE type, SSLs with dysplasia/carcinoma were significantly associated with adenomatous surface-patterns compared with SSLs without dysplasia (NICE type 2/3: 58.7% vs. 5.6%, p < 0.01). In the resection method, SSLs with dysplasia/carcinoma were significantly associated with ESD compared with SSLs without dysplasia (44.0% vs. 7.3%, p < 0.01). There was no difference in en bloc resection between the two groups. Regarding histologic margin status after endoscopic resection, SSLs without dysplasia were significantly associated with incomplete resection (positive or indeterminate margin) compared with SSLs with dysplasia/carcinoma (60.4% vs. 49.4%, p < 0.01).
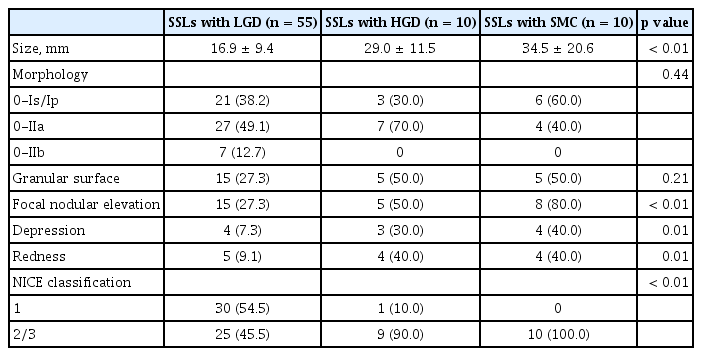
Endoscopic characteristics with regards to dysplasia degree in SSLs
The endoscopic characteristics with regards to dysplasia degree in SSLs are summarized in Table 3. Regarding size, SSLs with HGD and submucosal cancer (SMC) were significantly larger than SSLs with low-grade dysplasia (LGD) (29.0 ± 11.5 mm/34.5 ± 20.6 mm vs. 16.9 ± 9.4 mm, p < 0.01). Morphologically, there were no differences among the three groups. In the analysis of surface-changes, SSLs with HGD and SMC were significantly associated with focal nodular elevation (50.0%/80.0% vs. 27.3%, p < 0.01), depression (30.0%/40.0% vs. 7.3%, p = 0.01), and redness (40.0%/40.0% vs. 9.1%, p = 0.01) compared with SSLs with LGD. In NICE type, SSLs with HGD and SMC were significantly associated with adenomatous surface-patterns compared with SSLs without dysplasia (NICE type 2/3: 90.0%/100% vs. 45.5%, p < 0.01).
Clinical and endoscopic factors associated with dysplasia/carcinoma in SSLs
The results of the logistic regression analysis for clinical and endoscopic factors associated with dysplasia/carcinoma in SSLs are summarized in Table 4. On per-patient univariate analysis of clinical factors, advanced age, metabolic diseases, and high-risk adenomas were significantly associated with SSLs with dysplasia/carcinoma, but multiple SSLs were significantly associated with SSLs without dysplasia. On per-patient multivariate analysis of clinical factors, advanced age (odds ratio [OR], 1.03; 95% confidence interval [CI] 1.00–1.06; p = 0.08), metabolic diseases (OR, 1.79; 95% CI, 0.92–3.45; p = 0.09), high-risk adenomas (OR, 2.98; 95% CI, 1.25–7.11; p = 0.01) were significantly associated with SSLs with dysplasia/carcinoma.
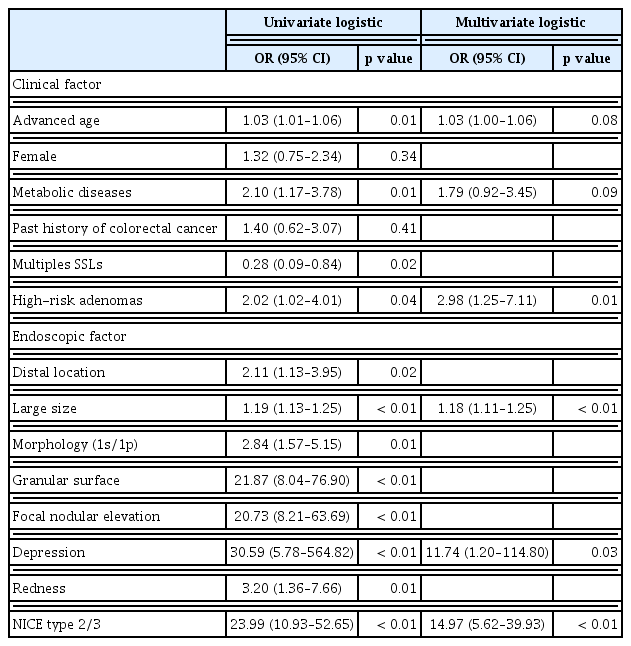
Logistic regression analysis (univariate and multivariate) for clinical and endoscopic factors associated with dysplasia/carcinoma in SSLs
On per-polyp univariate analysis of endoscopic factors, distal location, large size, polypoid morphology, granular surface, focal nodular elevation, depression, redness, and NICE type 2/3 were significantly associated with SSLs with dysplasia/carcinoma. On per-polyp multivariate analysis of endoscopic factors, large size (OR, 1.18; 95% CI, 1.11–1.25; p < 0.01), depression (OR, 11.74; 95% CI, 1.20–114.80; p = 0.03), and NICE type 2/3 (OR, 14.97; 95% CI, 5.62–39.93; p < 0.01) were significantly associated with SSLs with dysplasia/carcinoma.
The sensitivity, specificity, predictive value, and accuracy of the logistic model using four markers, including high-risk adenomas, large size, depression, and NICE type 2/3, which are valuable factors in the multivariate analysis for SSLs with dysplasia/carcinoma are shown in Table 5. This model showed a relatively low sensitivity of 72.0% (95% CI, 60.4–81.8) for identifying dysplasia/carcinoma within SSLs, but high specificity of 95.5% (95% CI, 91.4–98.1), positive predictive value of 87.1% (95% CI, 76.1–94.3), negative predictive value of 89.1% (95% CI, 83.8–93.1), and accuracy of 88.6% (95% CI, 84.0–92.2).
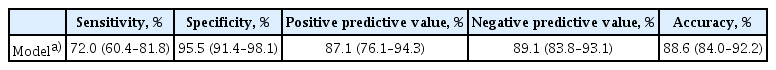
Sensitivity, specificity, predictive value, and accuracy of logistic model for SSLs with dysplasia/carcinoma
Representative endoscopic and pathological images of SSL with invasive carcinoma are shown in Figure 3.

A case of sessile serrated lesion with invasive carcinoma. (A, B) Endoscopic findings; (A) flat elevated lesion with some hyperemic and granular surfaces and (B) in near focus view, narrow-band imaging (NBI) international colorectal endoscopic classification (NICE) type 1/Kudo pit pattern (KPP) II-O (yellow arrows) and NICE type 2/3/KPP III/IV (blue arrows). (C, D) Gross findings of resected specimen; (C) 20 mm sized flat and elevated lesion with focal nodular elevation and (D) a depression in focal nodular elevation. (E–G) Histologic findings with hematoxylin and eosin staining (H&E) of the resected specimen; (E) transitional area from sessile serrated lesion to dysplasia (yellow arrow) and invasive carcinoma (blue arrow) (H&E, ×1), (F) high-power field of the right side of (E), serrated changes (yellow arrow) and architectural distortion like dilation and branching (blue arrow) of crypt in basal layer near muscularis mucosa (H&E, ×60), and (G) high-power field of the left side of (E), moderately differentiated adenocarcinoma invading the submucosal layer (blue arrows) (H&E, ×200).
DISCUSSION
SSLs with dysplasia/carcinoma can be easily missed or incompletely resected since most SSLs with dysplasia/carcinoma have subtle mucosal features covered with a sticky mucus [17,23], and eventually develop into interval cancer [28–30]. Therefore, the detection and complete resection of subtle mucosal features associated with dysplasia/carcinoma after mucus removal and careful endoscopic inspection is important for the prevention of interval cancer.
In the present study, the incidence of SSLs with dysplasia or carcinoma was 29.5% (75/254) which was similar or slightly higher than that reported in previous studies (2–30%) [4,7,8,31,32]. In addition, the incidence of SSLs with advanced histology, such as HGD and SMC, was high (7.9%; 20/254) compared with that reported in previous studies (0.4–5.6%) [8,20,33,34]. There are several reasons for the different incidences compared with previous studies, such as variable sample size, tertiary hospital and unavoidable selection bias of retrospective studies; however, the larger size of SSLs in this study is thought to be the most important reason. As observed, the mean size of all SSLs and SSLs with dysplasia/carcinoma were 12.9 mm and 20.9 mm in this study, respectively, but 9.5–15.0 mm and 14.3–20 mm in previous studies [17,20,33–35], respectively.
In analysis of endoscopic and pathological factors associated with dysplasia/carcinoma, distal colon, large size, polypoid morphology, surface-changes, no mucus cap, adenomatous surface-patterns, and histologically complete resection was significantly associated with SSLs with dysplasia/carcinoma, particularly large size, depression and NICE type 2/3 in multivariate analysis. Similar to previous studies [8,17–20,33,35–39], SSLs with dysplasia/carcinoma occurred more frequently in the proximal colon than in distal colon (52/254 [20.5%] vs. 23/254 [9.1%]) compared with SSLs without dysplasia. However, the risk of dysplasia was significantly higher in the distal colon than in the proximal colon (23/54 [42.6%] vs. 52/200 [26.0%], p = 0.02). This result was also observed in a previous study (81/213 [38.0%] vs. 81/319 [25.4%], p < 0.002) [34]. Moreover, similar tendencies were observed in previous studies (54.1% vs. 37.1% and 10.4% vs. 8.76%) [18,20]. In addition, in two studies regarding interval colorectal cancers in the Korean population, interval cancers frequently developed in the left colon (16/28 [57.1%] and 12/25 [48%], respectively) [40,41]. Although most SSLs take a long time to develop dysplasia, especially in the proximal colon, they in the distal colon may have different oncologic behaviors that are more aggressive. Therefore, SSLs with dysplasia/carcinoma frequently develop in the distal colon, while all SSLs found in the distal colon should be closely inspected for dysplasia. In the subgroup analysis of proximal lesions, previous studies had shown a slight predilection of dysplasia in SSLs found in the transverse colon [18,20], but our study showed similar results between SSLs with and without dysplasia in the transverse colon (7/52 [13.5%] vs. 19/148 [12.8%]).
SSLs with dysplasia/carcinoma in this study tended to be larger, which is consistent with findings from other studies [19,20,35]. Most SSLs with dysplasia had large size (70/75 [93.3%] in ≥ 10 mm and 25/75 [33.3%] in ≥ 20 mm) and < 6 mm diminutive SSLs with dysplasia was only 5.3% (4/75). Therefore, large size as a predictor of dysplasia in SSLs is important. Surface-changes similar to advanced adenomatous polyps were noted in SSLs with dysplasia/carcinoma. Previous studies have reported that the incidence of polypoid morphology, nodular component, double elevation, central depression, or redness within the lesions was higher in SSLs with dysplasia than those without [19,20,34,35]. In this study, polypoid morphology, granular surface, focal nodular elevation, depression, and redness were also found more frequently in SSLs with dysplasia/carcinoma. Therefore, SSLs with these surface-changes may be useful to accurately diagnose dysplasia and should be resected completely due to the high probability of rapid progression to invasive cancer. Although a mucus cap is frequently found in almost all SSLs [42,43] and may be one of the strongest markers of SSLs [17,20], its association with dysplasia is not established. A previous study reported that rims of debris/bubbles were more commonly found in SSLs without dysplasia [34], and the mucus cap in this study was significantly more frequent in SSLs without dysplasia than in those with dysplasia/carcinoma. These results suggest that mucus secretion decreases as SSLs without dysplasia are transformed into SSLs with dysplasia/carcinoma. Therefore, if SSLs are covered by a mucus cap, especially without surface-changes, the possibility of the presence of dysplasia or carcinoma in SSLs may be low.
NBI, which visualizes vessels and surface-patterns in detail, is generally considered to provide useful diagnostic information to differentiate hyperplastic polyps from adenomas. In a study by Murakami et al. [23] using the Japan NBI Expert Team classification, 95.5% of SSLs without dysplasia exhibited type 1 only, whereas 83.9% of SSLs with dysplasia/carcinoma had a combination of types 1 and 2 or 3 (p < 0.001); herein, using NICE, 94.4% of SSLs without dysplasia exhibited type 1 only and 58.7% of SSLs with dysplasia/carcinoma exhibited type 2 or 3 (p < 0.01). Therefore, NBI without magnification may aid in detecting dysplasia in SSLs. Magnifying colonoscopy is a more accurate tool for detecting dysplasia and analyzing Kudo pit patterns (type III, IV, or V) in SSLs [19,44], but it is difficult to use magnifying colonoscopy in most institutions.
En bloc resection of SSLs is important for precise histologic evaluation and the prevention of interval cancer. In a study by Tate et al. [33], en bloc resection rates in SSLs with and without dysplasia were 44.4% and 55.2%, respectively. The low en bloc resection rate in the above study was related to the type of resection using cold snare polypectomy and endoscopic mucosal resection (EMR) with high piecemeal resection rate in large tumors. In this study, most SSLs were resected by snare resection, including cold snare and conventional EMR; however, ESD was mainly used for SSLs ≥ 20 mm. The en bloc rate was similar between the two groups (96.0% vs. 96.1%). In this study, the high en bloc rate was due to the fact that most SSLs were < 20 mm in size and well captured by the snare. In case of large, flat lesions that were difficult to capture by the snare, en bloc resection was possible by ESD. But the histologically complete resection rate was significantly higher in SSLs with dysplasia/carcinoma than in those without dysplasia (50.6% vs. 39.6%, p < 0.01). These findings shows that SSLs without dysplasia commonly underwent snare resection due to their small size and low risk of cancer, however, SSLs with dysplasia/carcinoma underwent ESD owing to their large size and high-risk of cancer. Furthermore, the low histologically complete resection rate compared with the high en bloc rate was due to the fact that most SSLs underwent snare resection without sufficient margin. As a result, coagulation artifacts occurred at the tumor margin, resulting in an increase of the indeterminate resection margin.
Several studies have evaluated SSLs with advanced histology such as HGD and SMC, but the endoscopic characteristics were not included [19,33,34], while only few studies have investigated the endoscopic characteristics of SSLs with an advanced histology. In study by Murakami et al. [20], HGD and invasive carcinoma among SSLs were 4.1% (n = 19) and 1.5% (n = 7), respectively, and the morphologies of SSLs with invasive carcinoma were five sessile (71%) and two semi-pedunculated (29%) types. In review by Murakami et al. [17], the morphologies of SSLs with invasive carcinoma (n = 46) included 31 sessile (68%), 13 semipedunculated (28%), and two pedunculated (4%) types. However, these two studies did not evaluate the various endoscopic findings of SSLs with advanced histology. In this study, SSLs with advanced histology were significantly associated with large size, focal nodular elevation, depression, redness, and NICE type 2/3, similar to advanced adenomas. Therefore, in endoscopic resection of SSLs with these findings, en bloc resection is critical for precise pathologic examination and prevention of interval cancer.
This study has some limitations. First, this was a single tertiary-center, retrospective and nonrandomized study with relatively small number of samples and large size of SSLs; therefore, selection biases were unavoidable. Second, some S SLs may be endoscopically misdiagnosed as hyperplastic polyps and not be removed because flat polyps with diminutive size and NICE type 1 were generally diagnosed as hyperplastic polyps. However, the prevalence of SSLs in diminutive hyperplastic-appearing polyps was very low (0.6– 2.1%) [45,46], while in this study, all polyps with difficult differentiation were removed and pathologically evaluated. Third, the potential for interobserver variation among the pathologists may be developed. Ideally, all SSLs and hyperplastic polyps should be re-assessed in accordance with the WHO 2019 criteria by a subspeciality pathologist to ensure SSLs. However, this is very difficult in practice owing to heavy workload. Despite the limitations, this study has major contribution. Although most SSLs are located in the proximal colon and are an important cause of interval cancer in the proximal colon, the risk of dysplasia in the distal colon and the relationship between interval cancer and SSLs in the distal colon are not well known. This study suggests that SSLs in the distal colon had a higher risk of dysplasia and can be an important cause of interval cancer, as well as SSLs in proximal colon.
In conclusion, SSLs had a higher risk of dysplasia in the distal than proximal colon. SSLs with dysplasia or carcinoma usually develop in patients with co-existing metabolic diseases and high-risk adenomas. SSLs with large size, depression, and adenomatous surface-patterns, as well as in patients with high-risk adenomas, should be suspected dysplasia or carcinoma. Therefore, these clinical and endoscopic characteristics can aid in the diagnosis and management of SSLs with dysplasia.
KEY MESSAGE
1. Among 254 colorectal sessile serrated lesions (SSLs) endoscopically resected, the incidence of SSLs with dysplasia or carcinoma including 55 with low-grade dysplasia, 10 with high grade dysplasia and 10 with submucosal cancer was 29.5%.
2. SSLs had a higher risk of dysplasia in the distal than in proximal colon.
3. SSLs with large size, depression, and adenomatous surface-patterns, as well as in patients with high-risk adenomas, increased the risk of dysplasia/carcinoma.
Notes
CRedit authorship contributions
Peel Jung: data curation, writing - original draft; Hyung Wook Kim: conceptualization, funding acquisition, methodology, writing - original draft, writing - review & editing; Su Bum Park: formal analysis, methodology, project administration; Dae Hwan Kang: project administration, writing - review & editing; Cheol Woong Choi: project administration, visualization, writing - review & editing; Su Jin Kim: formal analysis, methodology, project administration, visualization; Hyeong Seok Nam: formal analysis, methodology, project administration, visualization; Dae Gon Ryu: data curation, formal analysis, project administration, visualization; Dong Hoon Shin: data curation, formal analysis; Joo Young Na: data curation, formal analysis; Mi Sook Yun: formal analysis
Conflicts of interest
The authors disclose no conflicts.
Funding
None