Diagnosis and management of acute colonic diverticulitis: results of a survey among Korean gastroenterologists
Article information
Abstract
Background/Aims
Some management strategies for acute colonic diverticulitis remain controversial in Korean real-world practice because their clinical features differ from those in the West. This study aimed to investigate the opinions of Korean physicians regarding the diagnosis and treatment of acute diverticulitis.
Methods
A web-based survey was conducted among gastroenterologists specializing on treating lower gastrointestinal disorders. The questionnaires concerned overall management strategies for colonic diverticulitis, including diagnosis, treatment, and follow-up.
Results
In total, 209 gastroenterologists responded to the survey. Less than one-fourth of the respondents (23.6%) answered that left-sided colonic diverticulitis is more likely to be complicated than right-sided colonic diverticulitis. Most respondents agreed that immunocompromised patients with diverticulitis have worse clinical outcomes than immunocompetent patients (71.3%). Computed tomography was the most preferred tool for diagnosing diverticulitis (93.9%). Approximately 89% of the respondents answered that they believed antibiotic treatment is necessary to treat acute uncomplicated diverticulitis. Most respondents (92.6%) agreed that emergency surgery is not required for diverticulitis with an abscess or microperforation without panperitonitis. Further, 94.7% of the respondents agreed that colon cancer screening is necessary in patients aged ≥ 50 years with diverticulitis after they have recovered from acute illness. Many respondents (71.4%) agreed that surgery for recurrent diverticulitis should be individualized.
Conclusions
Opinions regarding management strategies for colonic diverticulitis among Korean gastroenterologists were well agreed upon in some areas but did not agree well in other areas. Evidence-based guidelines that meet the practical needs of the Korean population should be developed.
INTRODUCTION
Colonic diverticulitis is one of the most common gastrointestinal diseases that significantly impacts the healthcare system. In the United States, the annual medical costs for diverticulitis exceed $5 billion [1]. Diverticulitis is more common in the West than in the East, but its incidence is increasing in Asian countries, including Korea [2,3]. Moreover, the incidence of diverticulitis has significantly increased among young patients in recent decades [4,5].
Although most cases of diverticulitis are uncomplicated, approximately 12% of patients develop complications, including abscesses, peritonitis, strictures, or fistulas [6]. Patients with perforations or abscesses may require surgical intervention and have a high mortality rate [4,7]. After the first episode of diverticulitis, the risk of recurrence is 22% at 10 years [4].
As our understanding of diverticulitis has increased over the past few decades, treatment strategies have shifted from aggressive and surgical treatment to less invasive and medical treatments [6]. Two multicenter randomized trials have identified no significant benefits of antibiotic treatment in patients with uncomplicated diverticulitis [8,9]. Furthermore, elective surgical resection for recurrent disease, based solely on the number of recurrences, is no longer recommended [10]. However, early aggressive treatment is recommended for high-risk patients, such as immunocompromised patients, who may develop serious clinical features [10–12].
However, despite the many studies conducted over a long period, some medical needs remain unmet, and several current management strategies are primarily based on expert opinions [6]. Further, as much of the evidence is based on studies conducted in the West, considerable gaps between the evidence and real-world clinical practice are expected in Asian countries, where the clinical features of acute colonic diverticulitis and the practice environments are different from those in the West. Therefore, the need to develop evidence-based guidelines for the medical management of acute colonic diverticulitis in Korea is emerging. We investigated the opinions of gastroenterologists in Korea regarding the diagnosis and medical management of patients with acute colonic diverticulitis in real-world practice.
METHODS
Survey
A cross-sectional, voluntary online survey was conducted between January 6 and February 21, 2022. The secure and protected platform SurveyMonkey was used in this survey. All members of the Korean Association for the Study of Intestinal Diseases, to which gastroenterologists mainly researching lower gastrointestinal tract disorders belong, were invited to participate via e-mail. The questionnaires on the SurveyMonkey platform were linked via email. To maintain anonymity, no identifiable information was requested from participants. Survey data were stored in a password-secured database.
The online survey was available in Korean and comprised seven domains to collect opinions on the overall medical management strategies for acute colonic diverticulitis as follows: respondent characteristics, clinical features of colonic diverticulitis, diagnosis, treatment, colorectal cancer screening, prevention, and recurrent disease. Both ‘yes’ and ‘no’ responses and multiple-response questions were used.
Before the survey, the questionnaires were reviewed, validated, and refined by independent experts for appropriateness and relevance. Sixteen main questions were included, and branching questions were added according to the responses. Thus, a maximum of 23 questions could have been answered. The English versions of the questionnaire are detailed in the Supplementary File. This study was approved by the Institutional Review Board of the Ewha Womans University Mokdong Hospital (IRB no. 2022-12-044). Informed consent was waived by the board.
Statistical analysis
Continuous variables are presented as means and standard deviations or medians with ranges. Categorical variables are expressed as numbers with proportions. The Kruskal–Wallis test was used to compare three or more groups. Statistical significance was set at p < 0.05. Statistical analyses were performed using the RStudio version 2022.2.2.485 (RStudio, Boston, MA, USA).
RESULTS
Characteristics of the respondents
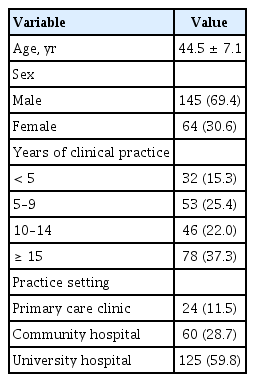
Table 1 presents the respondents’ characteristics. Altogether, 209 gastroenterologists responded to the survey, of whom 69.4% were male. The largest number of respondents (37.3%) had practiced for ≥ 15 years since becoming internal medicine specialists. Overall, 59.8% of the respondents were affiliated with university hospitals, 28.7% with community hospitals, and 11.5% with primary care clinics.
Opinions regarding clinical features
No predominant opinion was revealed regarding the severity of right- and left-sided colonic diverticulitis. In total, 43.1% of the respondents (84/195) answered that right-sided colonic diverticulitis had a greater risk of complicated disease, whereas 23.6% (46/195) answered that left-sided colonic diverticulitis had a greater risk. One-third (33.3%, 65/195) agreed that disease severity did not differ between right- and left-sided colonic diverticulitis (Fig. 1A).

Survey results of opinions on the clinical features of acute diverticulitis. (A) Opinions on disease severity of right and left colonic diverticulitis. (B) Opinions on prognosis of immunocompromised patients.
By contrast, more than two-thirds (71.3%, 139/195) agreed that immunocompromised patients with diverticulitis have worse clinical outcomes than immunocompetent patients (Fig. 1B).
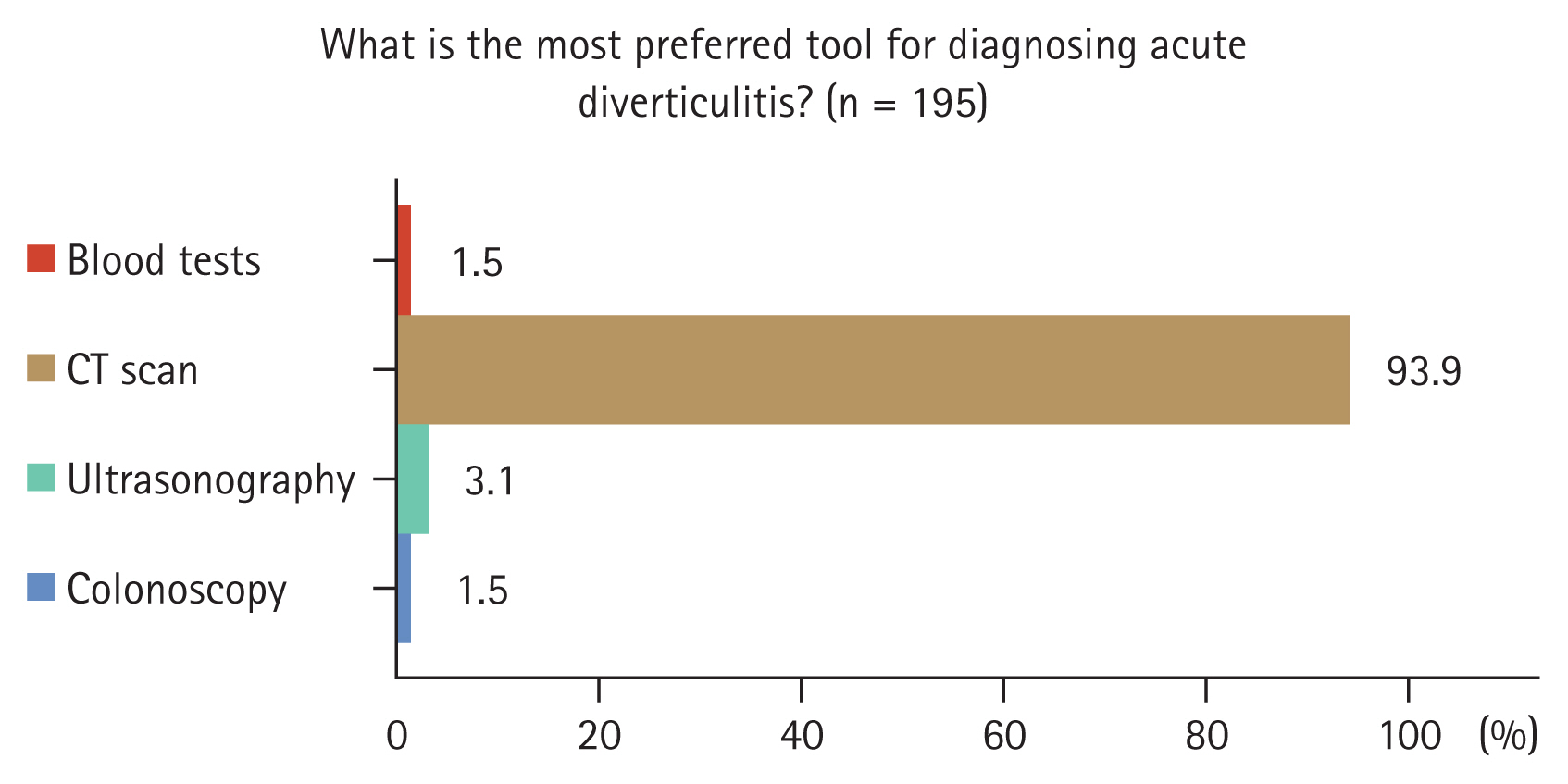
Opinions on diagnosis
Computed tomography (CT) was the most preferred tool for diagnosing diverticulitis by 93.9% of the respondents (183/195), followed by abdominal ultrasonography (3.1%, 6/195), colonoscopy (1.5%, 3/195), and blood tests (1.5%, 3/195) (Fig. 2).
In a multiple-response question regarding the measures taken to diagnose acute colonic diverticulitis in practice, spectively) answered that they had performed CT scans and blood tests, respectively. Fourteen of the 187 respondents (7.5%) answered abdominal ultrasonography, and eight of the 187 respondents (4.3%) answered colonoscopy for diagnosing diverticulitis in practice. Nine of the 187 respondents (4.9%) answered that they had transferred patients with suspected diverticulitis to a general or university hospital.
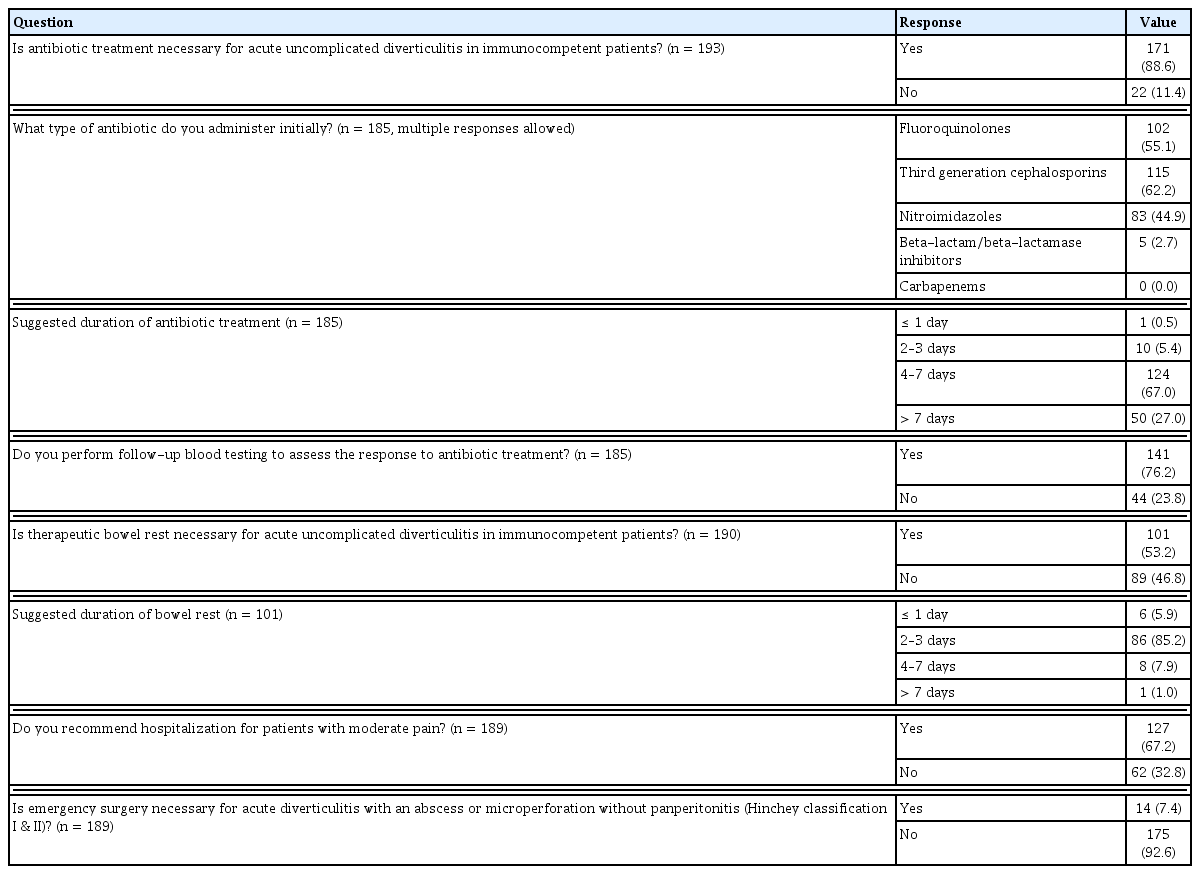
Opinions on treatment
Table 2 presents the survey results regarding opinions on the treatment of acute diverticulitis. Of the 193 respondents, 171 (88.6%) answered that antibiotic treatment is required for immunocompetent patients with uncomplicated diverticulitis. Only 11.4% (22/193) answered that antibiotic treatment is not necessary. The duration of antibiotic treatment was reported to be 4–7 days in 67.0% (124/185), > 7 days in 27.0%, 2–3 days in 5.4%, and 1 day in 0.5%. Fluoroquinolones, third-generation cephalosporins, and nitroimidazoles were the most preferred antibiotics by most respondents (multiple response question for the antibiotic regimen: 55.1% for fluoroquinolone [102/185], 62.2% for third-generation cephalosporins, 44.9% for nitroimidazoles, 2.7% for beta-lactam/beta-lactamase inhibitors, and none for carbapenems). In the multiple-response question regarding antibiotic regimens, 80/185 (43.2%) respondents selected only one antibiotic. Among these 80 respondents, 41 selected cephalosporins, 35 selected quinolones, 3 selected beta-lactam/beta-lactamase inhibitors, and 1 selected nitroimidazoles. The remaining 105/185 respondents (56.8%) selected two or more antibiotic options. Among the 105 respondents, the most common answers were cephalosporins and nitroimidazoles (36/105, 34.3%), followed by quinolones and nitroimidazoles (31/105, 29.5%).
Of the 22 respondents who answered that antibiotic treatment is not necessary for a previous question, 21 responded to the question of whether they prescribe antibiotics or not for immunocompetent patients with acute uncomplicated diverticulitis in their practice. Sixteen respondents (76.2%) reported that they administer antibiotics to patients with uncomplicated diverticulitis in their practice. The reasons for antibiotic treatment in real-world practice, despite the belief that antibiotic treatment is not necessary for patients with uncomplicated diverticulitis, were as follows: concerns regarding worsening of the disease course, 56.3% (9/16); antibiotic treatment had already been initiated by the first examining physician, 43.8% (7/16); the absence of complications could not be assured, 31.3% (5/16); and the possible harm of antibiotic treatment was not considered significant, 31.3% (5/16).
Of the 190 respondents, 101 (53.2%) responded that fasting and parenteral nutrition are necessary for immunocompetent patients with uncomplicated diverticulitis. Fasting duration was reported to be 2–3 days by 85.2% of the respondents (86/101), 4–7 days by 7.9%, 1 day by 5.9% (6/101), and > 7 days by 1.0% (1/101).
Many respondents (67.2%, 127/189) answered that they recommend hospitalization for patients with acute uncomplicated diverticulitis accompanied by moderate abdominal pain. The vast majority (92.6%, 175/189) reported that emergency surgery is not required for acute diverticulitis with an abscess or microperforation without panperitonitis (Hinchey classification I and II [13]).
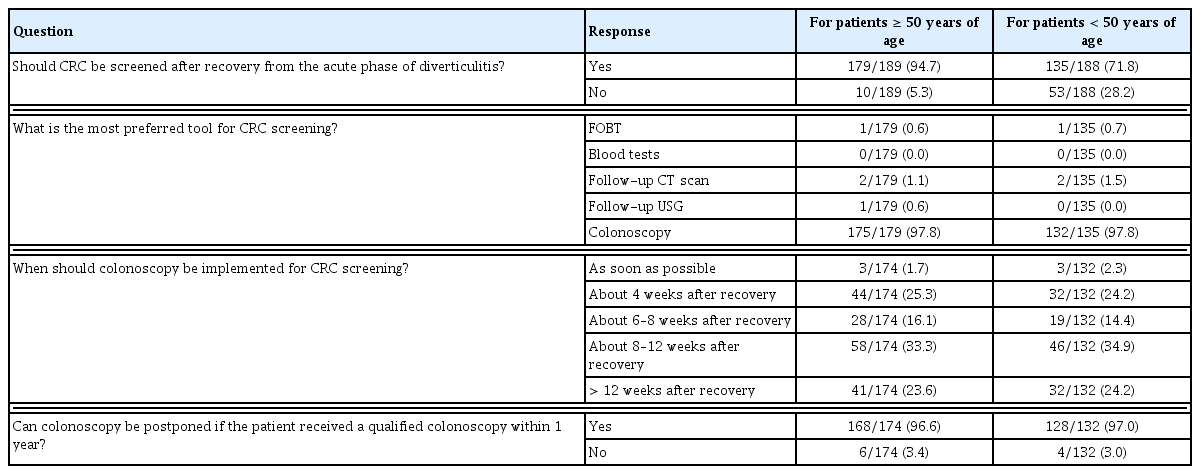
Opinions on colorectal cancer screening
Table 3 shows the survey results of the opinions on colorectal cancer screening after an episode of acute diverticulitis. Most respondents (94.7%, 179/189) agreed that patients with diverticulitis aged ≥ 50 years should be screened for colorectal cancer after they have recovered from an acute illness. The most preferred tool for colorectal cancer screening for patients aged ≥ 50 years was colonoscopy for 97.8% of the respondents (175/179), a follow-up CT scan for 1.1% (2/179), follow-up abdominal ultrasonography for 0.6% (1/179), and fecal occult blood test for 0.6% (1/179). The timing of colonoscopy was reported to be as follows: approximately 8–12 weeks after recovery, 33.3% (58/174); approximately 4 weeks after recovery, 25.3% (44/174); > 12 weeks after recovery, 23.6% (41/174); approximately 6–8 weeks after recovery, 16.1% (28/174); and as soon as possible after recovery from an acute illness, 1.7% (3/174). Most respondents (96.6%, 168/174) agreed that colonoscopy for colorectal cancer screening can be deferred in patients aged ≥ 50 years if the patient received a qualified colonoscopy within 1 year.
By contrast, less agreement was observed regarding the need for colonoscopy in patients aged < 50 years with diverticulitis. In total, 71.8% of the respondents (135/188) agreed that patients with diverticulitis in this age group should be screened for colorectal cancer after recovering from an acute illness. Similar to the answers to the previous question, the most preferred tool was colonoscopy (97.8% of the respondents). Regarding the timing of colonoscopy after the recovery of patients with diverticulitis, the largest number of the respondents (34.9%) preferred colonoscopy approximately 8 to 12 weeks after recovery from the disease.
Opinions on preventing recurrent diverticulitis
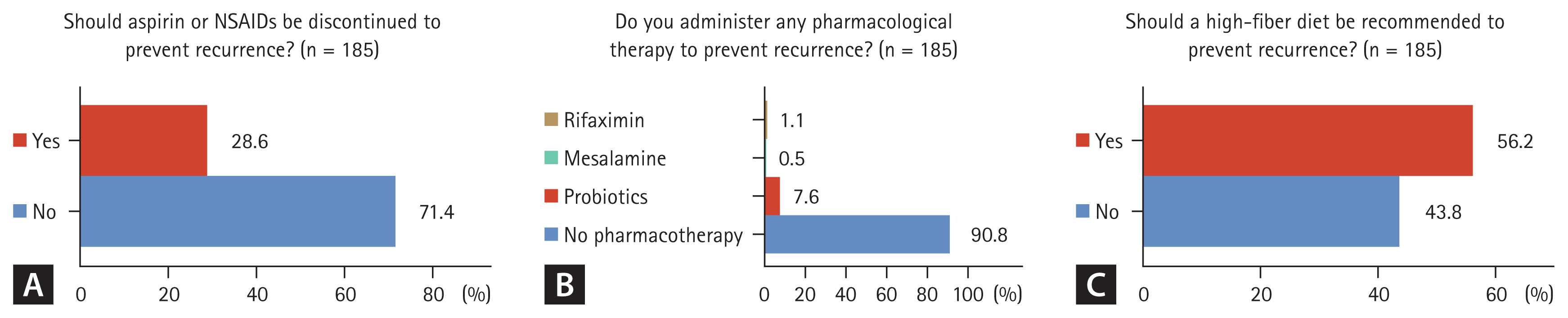
A total of 28.6% of respondents (53/185) agreed that non-steroidal anti-inflammatory drugs or aspirin should be discontinued to prevent recurrent diverticulitis, where- as 71.4% did not agree. Opinions regarding the use of pharmacotherapy to prevent recurrent diverticulitis were as follows: no pharmacological therapy, 90.8% (168/185); probiotics, 7.6%; rifaximin, 1.1%; and mesalamine, 0.5%. Opinions regarding the need for a high-fiber diet to prevent recurrence were mixed: 56.2% of the respondents (104/185) agreed that a high-fiber diet should be recommended, whereas 43.8% did not agree (Fig. 3).
Opinions on the management strategy for recurrent uncomplicated diverticulitis
A total of 22.7% of the respondents (42/185) answered that repeated medical treatment is favored for patients with multiple recurrences of acute uncomplicated diverticulitis, 6% answered that surgical treatment is favored, and 71.4% answered that treatment should be individualized, considering the number or frequency of recurrences and the patient’s medical condition. Regarding a more practical example of the need for elective surgery for a third recurrence of uncomplicated diverticulitis (assuming that the patient is not at a high risk for surgery), 34.6% of the respondents (64/185) agreed with planned surgery, whereas 65.4% did not agree. On the other hand, the need for elective surgery for the fourth recurrence of uncomplicated diverticulitis was agreed upon by 62.7% of the respondents (116/185) and not agreed upon by 37.3% (Fig. 4).
Subgroup analysis
Based on the respondents’ affiliations, no significant differences were detected in their opinions on antibiotic treatment and bowel rest for acute diverticulitis. By contrast, responses to the need for emergency surgery for acute diverticulitis with abscess or microperforation without pan-peritonitis differed significantly between the groups. While 30.0% of primary care practitioners (6/20) answered that emergency surgery is required, only 7.5% of community hospital physicians (4/53) and 3.4% of university hospital physicians (4/116) answered that emergency surgery would be required (p < 0.001). The preference for individualized treatment for multiple recurrences of acute diverticulitis was similar between the groups (approximately 70%). However, the need for elective surgery in patients with a fourth recurrence of uncomplicated diverticulitis differed significantly between the groups: 45.0% (9/20) of the respondents from primary care clinics, 53.8% from community hospitals (28/52), and 69.9% from university hospitals (79/113) (p = 0.031) (Supplementary Table 1).
Opinions on antibiotic treatment differed between groups of respondents with different numbers of years of practice. The need for antibiotic treatment in patients with uncomplicated diverticulitis was denied by 7.1% of the respondents with < 5 years of practice (2/28), 21.6% with 5–9 years of practice (11/51), 7.1% with 10–14 years of practice (3/42), and 8.3% with ≥ 15 years of practice (6/72) (p = 0.067). The suggested duration of antibiotic treatment differed significantly between the groups. Those who responded that the duration of antibiotic treatment was > 7 days were 7.1% of those with < 5 years of practice (2/28), 23.9% of those with 5–9 years of practice (11/46), 47.6% of those with 10–14 years of practice (20/42), and 24.6% of those with ≥ 15 years of practice (17/69) (p = 0.012). In addition, a relatively high agreement was observed for the need for emergency surgery for acute diverticulitis with an abscess or micro perforation without panperitonitis in respondents with < 5 years of practice. The need for emergency surgery was agreed upon by 17.9% of the respondents with < 5 years of practice (5/28), 6.1% with 5–9 years of practice (3/49), 0% with 10–14 years of practice (0/42), and 8.6% with ≥ 15 years of practice (6/70) (p = 0.045) (Supplementary Table 2).
The results of the questionnaire and relevant guideline recommendations or evidence are summarized in Supplementary Table 3.
DISCUSSION
In this study, we surveyed the diagnosis and management of acute colonic diverticulitis among gastroenterologists with varying levels of practical experience at various institutions. Opinions agreed well in some areas of management but not in others.
No dominant opinion has emerged regarding the disease severity between right- and left-sided colonic diverticulitis. More respondents answered that right-sided colonic diverticulitis is likely to be more complicated than left-sided colonic diverticulitis. However, previous studies have reported that patients with left-sided colonic diverticulitis are more likely to have complicated disease, postoperative morbidities, longer hospital stays, and recurrent disease than those with right-sided colonic diverticulitis [14–17]. In a recent systematic review and meta-analysis that included 21 studies and 2,811 patients with uncomplicated right-sided colonic diverticulitis who received conservative treatment, the pooled treatment failure rate was 2.5% [18]. This discrepancy may be because our survey was conducted among gastroenterologists in Korea who have relatively limited clinical experience with left-sided colonic and complicated diverticulitis requiring surgical treatment. Because right-sided colonic diverticulitis is considerably more common, with an incidence of 77.2–88.3% in East Asia [19–21], physicians might have relatively little experience with left-sided colonic diverticulitis. However, as Korea has gradually become more westernized, the incidence of left-sided colonic diverticulitis is expected to increase because acquired and environmental factors affect its risk [22]. Indeed, a Japanese study has reported a steady increase in the incidence of left-sided diverticulitis over the past few decades, from 4% in 1998 to 36% in 2009 [23]. In nine recent studies in Asian countries, including Korea, the ratio of left- to right-sided colonic diverticulitis was 0.08:1.0. However, combining the results of these studies totaled to 2,542 cases of right-sided colonic diverticulitis and 1,888 cases of left-sided colonic diverticulitis, with a left–right ratio of 0.62 [15,17,23–29]. As left-sided colonic diverticulitis is no longer uncommon in Asians, physicians should be aware that such patients are more likely to present with severe or complicated diseases and have poorer outcomes than those with right-sided colonic diverticulitis.
Notably, approximately 90% of gastroenterologists have reported that antibiotic treatment is necessary in immunocompetent patients with uncomplicated diverticulitis. This result reflects the fact that antibiotic treatment is widely implemented in patients with uncomplicated diverticulitis in real-world practice, although studies have demonstrated that antibiotic treatment does not result in better clinical outcomes [8,9]. Long-term follow-up data from antibiotic trials have also demonstrated no significant differences in recurrence, complications, surgery for diverticulitis, or colorectal cancer between patients who were treated with antibiotics and those who were not [30]. Moreover, antibiotic treatment for uncomplicated right-sided colonic diverticulitis, which is predominant in Eastern populations, was not associated with better clinical outcomes [31,32]. Our results revealed that 88.6% of the respondents answered that antibiotic treatment is necessary for immunocompetent patients with uncomplicated diverticulitis, and 76.2% of the respondents who did not agree with antibiotic treatment answered that they implemented antibiotic treatment in real-world practice for various reasons. Considering these survey results, it seems that almost all patients with diverticulitis in Korea are treated with antibiotics in real-world practice. Although the question may be complicated, if antibiotics were used for various reasons by physicians who did not agree with the necessity of antibiotic treatment, it would be because they believed that antibiotics were necessary. Concerns regarding the complications and embarrassment that could arise in the case of disease exacerbation, even if rare, may be the main reason for antibiotic treatment. Additionally, although not specified in this questionnaire, there may be an expectation of reducing the symptoms of diverticulitis through antibiotic treatment. Although more than half answered that they administer antibiotics for < 7 days, more experienced physicians were more likely to prescribe antibiotics for a longer time (33.3% of the respondents with ≥ 10 years of practice vs. 17.6% of the respondents with < 10 years of practice answered the duration of antibiotic treatment as ≥ 7 days). Moreover, the agreement rates for the need for bowel rest and hospitalization for acute uncomplicated colonic diverticulitis were 53.2% and 67.2%, respectively. These results suggest that Korean gastroenterologists appear to adopt safer management strategies than the current guideline recommendations. Although a survey conducted in the Netherlands has revealed that the need for antibiotic therapy for uncomplicated diverticulitis was agreed upon by 10% of surgeons [33], another multinational survey study has reported that the need for antibiotic therapy for uncomplicated diverticulitis was agreed upon by approximately 50% of surgeons [34]. Additionally, a real-world multicenter prospective observational study on the treatment of acute diverticulitis conducted in Italy demonstrated that antibiotic treatment was administered to 89.3% of patients with uncomplicated diverticulitis, reflecting the considerable gap between evidence, surveys, and clinical practice [35]. Ultimately, the gap between theory and practice in antibiotic treatment revealed in this Korean survey indicates that the use of empirical antibiotics in actual practice may not decrease in the near future even if evidence-based clinical guidelines are presented. Therefore, efforts are required to narrow these gaps.
Most respondents agreed that non-operative medical treatment can be performed first for diverticulitis with an abscess or microperforation unless it is accompanied by generalized peritonitis. This treatment strategy is consistent with the current guideline recommendations. Several guidelines recommend antibiotic therapy as the first-line treatment for diverticular abscesses, and abscesses of > 3–5 cm can be treated with drainage [11,12,36]. However, our subgroup analysis revealed that 17.9% and 30.0% of respondents with < 5 years of practice and who were primary care practitioners, respectively, agreed to emergency surgery for diverticulitis with an abscess or microperforation. These results indicate that opinions regarding the treatment of complicated diverticulitis may vary according to the physician’s experience and practice setting.
Most respondents agreed that screening for colon cancer is required after recovery from acute diverticulitis, which is consistent with the current guideline recommendations. Although the risk of underlying colonic neoplasia, including advanced adenoma or carcinoma, is low in patients with diverticulitis, several guidelines recommend performing a colonic evaluation after an acute episode of diverticulitis because overlooked colonic neoplasia can lead to serious and fatal consequences [10–12,36]. In particular, advanced age and complicated diverticulitis are associated with a high risk of colonic malignancies. In a recent systematic review and meta-analysis, 1.67% of the patients with CT-diagnosed diverticulitis had colonic malignancies. Meanwhile, the pooled prevalence of colonic malignancy was 1.22 and 6.14% in patients with uncomplicated and complicated diverticulitis, respectively, indicating a significant difference [37].
The contrast in agreement on the need for surgery in patients with third and fourth recurrences of acute diverticulitis was remarkable. The recommendation for elective surgical resection for a third recurrence was opposed by approximately two-thirds of the respondents, whereas surgical resection for a fourth recurrence was favored by approximately two-thirds. Moreover, the responses varied according to the subgroups of respondents’ affiliations and years of practice. Therefore, difficulties are expected in making surgical decisions regarding multiple recurrent diseases. Previous trials on elective sigmoid resection for recurrent left-sided colonic diverticulitis have demonstrated improved quality of life in patients who underwent elective surgical resection compared to those who did not [38,39]. Further, long-term outcome data of surgical resection for recurrent diverticulitis have demonstrated that patients who received surgical treatment had an increased quality of life at the 5-year follow-up compared to those who received conservative treatment, and 46% of patients in the conservative group ultimately required surgical treatment [40]. However, considering that surgical resection carries an inherent risk of complications and that most cases of right-sided diverticulitis have a benign disease course, surgical treatment for recurrent uncomplicated right-sided diverticulitis should be further investigated.
This study has some limitations. First, each question was not presented in detail, so the practice patterns were crudely investigated. Second, because some respondents did not respond to certain questions, we could not collect all their opinions. Third, most respondents were affiliated with hospitals that provided inpatient care, and many were affiliated with academic hospitals. These factors may have influenced the survey responses. Fourth, colorectal surgeons, general practitioners, and family physicians were not included in the survey. However, most studies on acute colonic diverticulitis to date have been conducted in Western countries by surgeons, and data on Eastern populations and the opinions of gastroenterologists are scarce. The results of this survey elucidate the current status of medical management strategies for acute colonic diverticulitis from the perspective of gastroenterologists.
In conclusion, our survey of management strategies for acute colonic diverticulitis revealed gaps between theory and clinical practice. Less than one-fourth of the respondents agreed that left-sided diverticulitis is likely to be more complicated than right-sided diverticulitis, whereas antibiotic treatment for acute uncomplicated diverticulitis was agreed upon by most respondents. Evidence-based clinical practice guidelines for overall management strategies, including diagnosis, medical and surgical treatment, follow-up, and prevention, need to be developed.
KEY MESSAGE
1. In our survey, approximately 89% of the Korean gastroenterologists answered that antibiotic treatment is necessary for immunocompetent patients with uncomplicated diverticulitis, reflecting a considerable gap between evidence and clinical practice.
2. More than 90% of respondents agreed that conservative treatment can be performed first for diverticulitis with abscesses or microperforation and that colon cancer should be screened after recovery from acute illness, which is consistent with the current guideline recommendations.
3. Many respondents answered that treatment strategies for recurrent diverticulitis should be individualized.
Notes
CRedit authorship contributions
Jae Gon Lee: data curation, formal analysis, writing - original draft; Yong Eun Park: methodology, validation; Ji Young Chang: methodology, validation; Hyun Joo Song: methodology, validation; Duk Hwan Kim: methodology, validation; Young Joo Yang: methodology, validation; Byung Chang Kim: methodology, validation; Shin Hee Lee: methodology, validation; Myung-Won You: methodology, validation; Seong-Eun Kim: conceptualization, writing - review & editing, supervision
Conflicts of interest
The authors disclose no conflicts.
Funding
None