Metabolic syndrome awareness in the general Korean population: results from a nationwide survey
Article information
Abstract
Background/Aims
Metabolic syndrome (MetS) raises the risk of cardiovascular disease and type 2 diabetes. An awareness of MetS is vital for early detection and proactive management, which can mitigate the risks associated with MetS. Therefore, our study aimed to investigate the level of awareness of MetS among the Korean population.
Methods
We conducted a nationwide survey between January and February 2023 among a representative sample of the Korean population using an online survey. Information regarding the awareness of MetS and its risk, the importance of lifestyle modification, and health behavior were collected. The question about the awareness of MetS was “How much do you think you know about MetS?” and there were five answers: 1) I know very well, 2) I know well, 3) I know a little, 4) I do not know, and 5) I have no idea. The high-awareness group was defined as those who answered that they knew very well or well.
Results
Among 1,000 participants (mean age, 45.7 ± 13.2 yr), 29% were unaware of MetS, and only 20.8% had high awareness. The high-awareness group was significantly more knowledgeable about lifestyle modifications and demonstrated better health behaviors. After adjustment for possible confounding factors, younger age, low household income, and absence of comorbidity were independently associated with a lack of awareness regarding MetS.
Conclusions
The high-awareness group showed greater knowledge of the importance of lifestyle modifications and better health behaviors regarding MetS. The findings highlight the need for improved public education and awareness programs regarding MetS.
INTRODUCTION
Metabolic syndrome is recognized globally as a significant public health concern. It is characterized by a cluster of interconnected metabolic dysfunctions, including insulin resistance, hypertension, and dyslipidemia, that collectively increase the risk of cardiovascular disease (CVD) and type 2 diabetes [1,2]. Notably, its prevalence is increasing globally. In South Korea, this escalation in the prevalence rate of metabolic syndrome is attributed to rapid urbanization, an aging population, and lifestyle changes [3,4]. Despite this increasing prevalence, research by Scuteri et al. (2015) and others has revealed a general lack of public awareness of this syndrome [5]. This paucity of knowledge can have severe implications on health outcomes, as understanding the condition is crucial for encouraging individuals to engage in preventive measures such as dietary modifications and regular exercise [6]. Awareness is the initial step towards promoting behavioral changes and preventive actions, and risk-informed individuals are more likely to make lifestyle modifications to reduce their risk of developing metabolic syndrome [7]. Increased awareness can further facilitate the early detection and management of the syndrome, thereby reducing the potential for developing severe complications such as CVD and type 2 diabetes [8].
Despite this alarming situation in Korea, empirical evidence on the population’s understanding of metabolic syndrome remains limited [4]. To address this gap, our study aimed to investigate the level of awareness about metabolic syndrome among the Korean population.
METHODS
Study design and data collection
This cross-sectional online survey was conducted between January and February 2023. Excluding the study design, the survey process was outsourced to MegaResearch (Seoul, Korea). The estimated target population (aged ≥ 20 yr) in December 2022 was 37,121,412. To represent Korean adults aged between 20 and 69 years, the survey population (n = 1,000) was selected using a stratified systematic sampling method, considering gender (men/women), age (20–29, 30–39, 40–49, 50–59, and 60–69 yr), and place of residence (eight metropolitan cities and eight non-metropolitan cities). The study was conducted through online interviews by sending web survey page links to randomly selected individuals from a panel of members of a subscription-based professional survey company. The respondents answered the web questionnaire using a mouse and keyboard, and the entered responses were automatically collected and managed on a data server. The web questionnaire was written using web programming languages that closely resemble offline survey procedures. Non-responses were systematically eliminated by the web page, which was programmed to not allow respondents to proceed to the subsequent page if a response was missed. Survey execution and management were conducted by the research company, and progress was monitored in real-time during the online survey.
Study population
The study population was derived from the target population, estimated by stratification based on gender, age, and place of residence. Eligible participants were aged between 20 and 69 years, agreed to participate in the survey, and answered the questions after understanding them. Responses completed up to the last question were considered valid. We excluded the following participants: 1) those aged < 20 years or ≥ 70 years, 2) those with significantly low online accessibility, 3) those who did not agree to participate in the survey, 4) those who failed to respond to the last question, and 5) those of a specific gender and age group that exceeded the assigned survey ratio during the survey.
Questionnaire
Participant eligibility was determined on the basis of age, gender, and place of residence, which were the initial questions asked in the survey (Supplementary Material). The main body of the survey was divided into three sections:
1) The first section gathered demographic data, such as educational attainment; income; type of residence; marital status; and health status, including the presence of hypertension, dyslipidemia, diabetes, central obesity, CVD, cerebrovascular disease, social history of alcohol consumption and smoking habits, and family history of CVD.
2) The second section assessed participants’ awareness of metabolic syndrome. Participants were asked, “How much do you think you know about metabolic syndrome?” with five potential responses: (1) I know very well, (2) I know well, (3) I know a little, (4) I do not know, and (5) I have no idea. These responses were based on subjective judgments of the participants.
3) The third and final section explored understanding the importance of lifestyle modifications and health behaviors in relation to metabolic syndrome. For each lifestyle modification category (calorie intake control, exercise, weight reduction, smoking cessation, and medical treatment [i.e., the need for medical consultation or intervention]), participants rated the importance on a 5-point scale from “very necessary” to “not necessary at all.” For health behavior within the last three years, participants measured health parameters, including body weight, waist circumference, and blood pressure. Additionally, details on specific lifestyle modifications, such as regularly measuring blood pressure, getting adequate sleep, following a low-salt diet, and exercising regularly, were gathered.
Participants who responded that they knew about metabolic syndrome “very well” or “well” were categorized as the high awareness group, while those who responded with “I know a little”, “I do not know”, or “I have no idea” were classified as the low awareness group.
Ethics
Personal information was not collected during the online survey. The local Institutional Review Board of Gachon University Medical Center approved this study (GFIRB2023-084) and waived the requirement for written informed consent.
Statistical analysis
All categorical data are presented as frequencies and percentages. Pearson’s chi-squared test was used to compare categorical variables. A linear-by-linear association was employed to discern trends in clinical characteristics based on the responses. Additionally, a univariate analysis was conducted, followed by a multivariate logistic regression analysis to evaluate the risk of lack of awareness of metabolic syndrome while accounting for individual risk factors. Variables that showed a significant predictive value (p < 0.05) in univariate analysis were subsequently incorporated into the regression analysis. The threshold for statistical significance was set at p < 0.05. All statistical analyses were performed using the SPSS software (version 22.0; IBM Corp., Armonk, NY, USA).
RESULTS
Characteristics of the study population
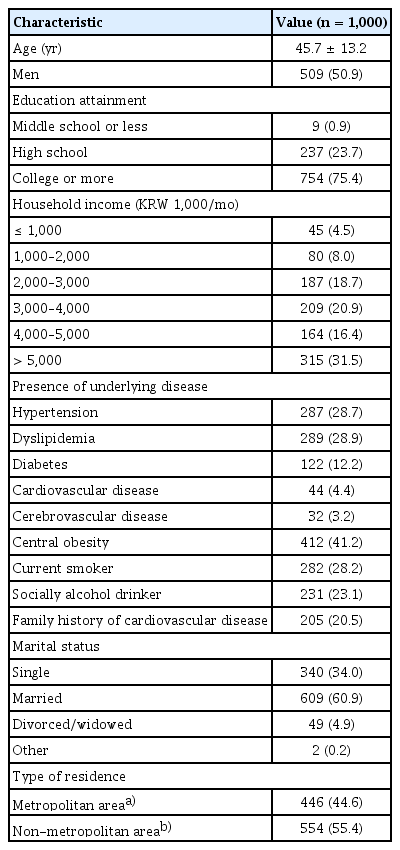
A total of 1,000 selected participants completed an online interview based on systematic stratification sampling. The study participants were evenly distributed according to age, gender, and place of residence. Table 1 presents the characteristics of the study population. The mean age of the study population was 45.7 ± 13.2 years (range, 20–69 yr), and approximately half of the participants were men (50.9%). The majority of participants had attained a college education or higher (75.4%), with a smaller percentage having a high school education (23.7%), and less than one percent (0.9%) having middle school education or less. In terms of income, 31.5% had a household income of more than 5,000 (KRW 1,000/mo), while 4.5% had an income of 1,000 (KRW 1,000/mo) or less. The remaining individuals fell within these income brackets. Regarding underlying health conditions, the most common underlying disease was central obesity (41.2%), followed by dyslipidemia (28.9%), hypertension (28.7%), and diabetes (12.2%); CVD and cerebrovascular disease were present in 4.4% and 3.2% of participants, respectively. Of the participants, 28.2% were current smokers and 23.1% were social alcohol drinkers. Regarding marital status, 60.9% of the participants were married, 34.0% were single, and 4.9% were divorced or widowed.
Awareness regarding metabolic syndrome
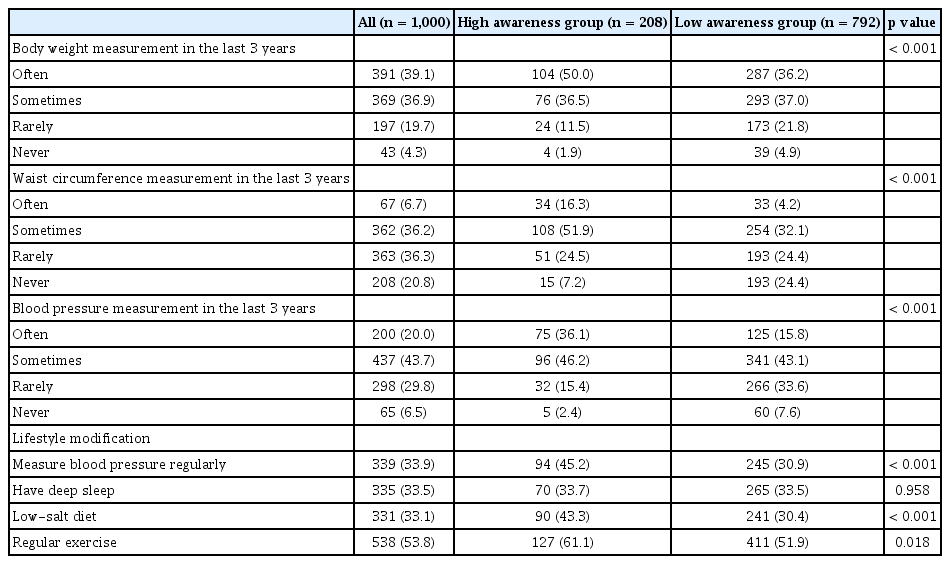
Approximately 80% of the participants listed “I do not know,” “I have no idea” or “I know a little” about metabolic syndrome (Fig. 1). A mere 4.2% of participants, which corresponds to 42 individuals, answered that “I know very well.” Further, an additional 16.6% of the population, equivalent to 166 participants, reported that “I know well.” Three-quarters (78.8%) of the participants answered that they had heard of metabolic syndrome in the previous year (Fig. 2). The most common sources of information were television and radio (40.4%) followed by the internet or YouTube (28.9%); other sources included friends, relatives, hospital care staff, newspapers, and magazines.
The extent to which participants know about metabolic syndrome. Question: How much do you think you know about metabolic syndrome?

Awareness of metabolic syndrome and the awareness pathways. Question: Have you ever heard of metabolic syndrome?
Notably, awareness of metabolic syndrome varied significantly across different demographic parameters, such as in age group, education level, household income, presence of underlying disease, and marital status (Table 2). Among the different age groups, the highest awareness levels were observed in individuals aged 60–69 years and 50–59 years (percentage of those who answered “I know very well” or “I know well”), while the youngest age group (20–29 yr) showed the lowest awareness levels (percentage of those who answered “I have no idea” or “I do not know”). Additionally, awareness increased with an increase in the level of education and household income. Participants with comorbid conditions demonstrated a higher level of awareness of metabolic syndrome. Married individuals exhibited a higher level of awareness, whereas those living alone exhibited a lower level. Additionally, respondents with a high level of metabolic syndrome awareness tended to live in the eight major metropolitan cities.
Understanding the importance of lifestyle modifications and health behaviors in metabolic syndrome
Table 3 and Supplementary Figure 1 present differences in the awareness of the general population regarding the importance of lifestyle modifications in relation to metabolic syndrome. Participants were divided into two groups according to their level of awareness: a high-awareness group (n = 208) and a low-awareness group (n = 792). Significantly different distributions between the high- and low-awareness groups were observed in each category, as indicated by p values < 0.001. For calorie intake control, 59.1% of the high awareness group viewed it as “very necessary,” compared to only 30.3% in the low awareness group. Similar trends were observed in the exercise, weight reduction, smoking cessation, and medical treatment categories, with higher percentages of the high awareness group rating these interventions as “very necessary.” Interestingly, the highest levels of “very necessary” responses across both groups were observed for weight reduction, with 63.5% of the high awareness group and 50.9% of the low awareness group agreeing. Even in the high awareness group, only 50.5% perceived medical treatment as “very necessary”, highlighting a lack of understanding of the importance of medical treatment among individuals with metabolic syndrome.
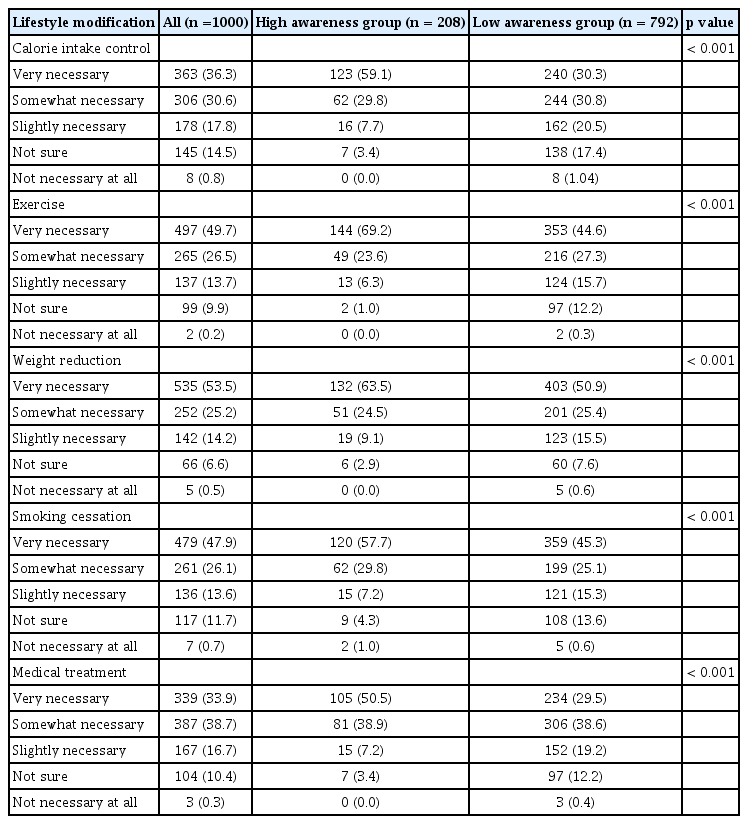
Differences in awareness of the importance of lifestyle modifications for metabolic syndrome in the general population according to awareness
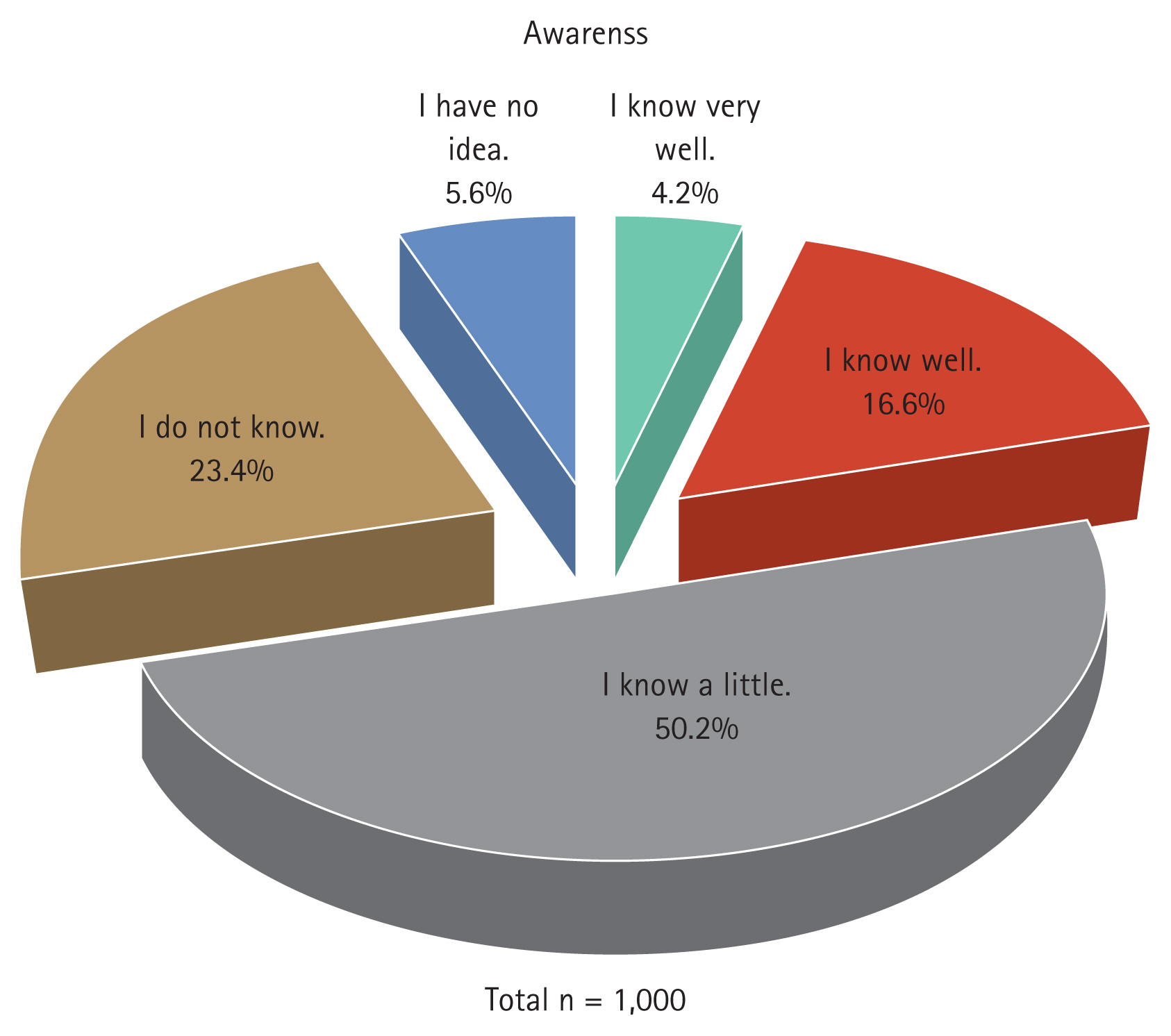
Table 4 and Supplementary Figure 2 detail differences in health behaviors of the general population related to metabolic syndrome between the two groups. In the high awareness group, a higher proportion of individuals “often” measured their body weight (50.0%) compared to the low awareness group (36.2%). Similarly, the high awareness group more frequently measured their waist circumference and blood pressure, with 16.3% and 36.1% doing so “often” compared to 4.2% and 15.8% in the low awareness group, respectively. These differences are statistically significant, as indicated by p values < 0.001. In terms of lifestyle modifications, more participants in the high awareness group regularly measured blood pressure (45.2% vs. 30.9%), followed a low-salt diet (43.3% vs. 30.4%), and exercised regularly (61.1% vs. 51.9%) compared to the low awareness group. These differences were also statistically significant (p < 0.05), excluding the practice of ensuring a restful sleep, where no significant difference was observed between the two groups (p = 0.958).
Risk factors for lack of awareness of metabolic syndrome
The univariate analysis in Table 5 showed that the following variables were associated with a lack of awareness about metabolic syndrome (“I do not know” and “I have no idea”) in the general population: increasing age (from 20s to 60s), a below college level of education, a household income < 2,000 (in 1,000 KRW/mo), absence of comorbidity, and single-person households.

Factors associated with lack of awareness (I do not know or I have no idea) about metabolic syndrome in the general population
After adjusting for possible confounding factors in the multivariate analysis, each decade increase in age from the 20s to the 60s was associated with a 25% decreased hazard (odds ratio of 0.75) for lack of awareness of metabolic syndrome. This indicates that awareness increases with age. Lower household income (< 2,000 in 1,000 KRW/mo) was associated with a 2.13-fold increased risk of lack of awareness, suggesting that lower income significantly contributes to decreased awareness. The absence of comorbidities was also independently associated with a lack of awareness, increasing the risk by 56% (odds ratio, 1.56). However, having a below college level of education and single-person households had no statistically significant associations toward lower awareness.
DISCUSSION
Our recent cross-sectional web-based survey offers pivotal findings regarding the awareness level of metabolic syndrome within the adult Korean population, specifically among those aged 20–69 years. Although a stratified systematic sampling approach was employed to ensure a wide representation of the demographic groups, the data indicated a substantial awareness gap regarding metabolic syndrome among the respondents. Additionally, this study underscored the correlation between level of awareness and participant recognition of the importance of lifestyle alterations to enhance health. Individuals with higher awareness levels demonstrated superior comprehension and involvement in behaviors that promote better health. Interestingly, specific risk factors such as younger age, lower household income, and lack of comorbid conditions were found to be associated with reduced awareness. This knowledge could help shape targeted educational strategies to boost awareness and understanding of metabolic syndrome.
Metabolic syndrome, which includes a cluster of interconnected factors, such as insulin resistance, hypertension, and dyslipidemia, is recognized as a major worldwide health concern [9,10]. Globally, the prevalence of metabolic syndrome is increasing, with significant increases occurring in certain regions and specific ethnic groups. In the US, the rate of metabolic syndrome is escalating faster in Asian and Hispanic adults than in other racial groups [11]. In the Asia-Pacific region, the prevalence of metabolic syndrome varies from 11.9 to 49.0% in the adult population, with a notable increase in East Asia [12]. Notably, the metabolic dysfunction associated with metabolic syndrome poses a significant risk of developing CVD [13]. Moreover, each additional metabolic syndrome component has been found to increase the risk of a significant cardiovascular events by 22% [14].
Building on this global perspective, understanding regional differences and the impact of lifestyle and socioeconomic changes on the prevalence of metabolic syndrome is of paramount importance. A range of factors, including obesity, diet, physical activity, and socioeconomic influences, contribute to the development of metabolic syndrome [1]. Countries experiencing swift economic changes often see drastic lifestyle changes and subsequent shifts in the incidence and prevalence of chronic diseases [15]. Economic growth was paralleled by a significant nutritional transition, as consumption of processed foods and animal products increased, intake of plant foods decreased, and a shift occurred in the primary cause of death from infectious to CVDs [16]. Although previous studies have investigated the progression of metabolic syndrome in South Korea, certain aspects remain unaddressed. The prevalence of the syndrome was found to have increased from 24.9% in 1998 to 30.52% in 2013, but alterations in lifestyle and socioeconomic factors were not considered, and the time period investigated was relatively short [17,18]. In contrast, a more recent study examined changes in the prevalence of metabolic syndrome from 2001 to 2020, accounting for alterations in the components of metabolic syndrome and related lifestyle factors, using data from the Korean National Health and Nutrition Examination Survey (KNHANES) [19].
In our study, as we delved into socioeconomic influences and changing lifestyle patterns, it became clear that enhanced awareness and recognition of metabolic syndrome are crucial. The increasing global prevalence of metabolic syndrome underscores the importance of recognizing its severity and the need for effective management and prevention. Despite South Korea’s status as a developed country, there remains an urgent need to enhance awareness of this prevalent condition [20]. The situation in South Korea is pressing, with studies revealing a marked lack of awareness of metabolic syndrome and its connection with lifestyle and socioeconomic factors [17]. Cultural influences can significantly affect awareness, as established in previous research, thereby stressing the need for tailored educational initiatives [21]. In China, a considerable number of adults remain unaware of their metabolic risk factors [22], further emphasizing the need for easily understandable measures like the “A Body Shape Index” and the “Waist to Height Ratio” [23]. Moreover, studies have highlighted that certain lifestyle risk factors, such as with sedentary and low activity jobs, pose significant risks for developing total and central obesity, particularly in middle-aged male workers [24]. This knowledge substantiates the importance of raising awareness of these factors as part of an overall strategy to combat metabolic syndrome. Our study illustrates that awareness directly influences an individual’s commitment to lifestyle modifications to manage metabolic risks. Those with higher awareness perceived these changes as more vital and engaged more frequently in health-promoting behaviors than their lower awareness counterparts.
Having discussed the role of awareness in managing metabolic syndrome, our study examined the specific factors contributing to this lack of awareness. Remarkably, our study found an association between young age, low household income, absence of comorbidities, and lack of awareness of metabolic syndrome. There are several possible reasons for this observation. Young individuals may perceive themselves as invincible to health conditions such as metabolic syndrome, which is often associated with older age groups. Consequently, they may not actively seek information about health risks. People with lower incomes may face more pressing immediate needs or lack access to resources that facilitate health education, thereby limiting their exposure to vital health information. Finally, those without preexisting health conditions might not interact as frequently with the healthcare system, which is a significant source of health risk education. These findings underline the need to target health education initiatives towards at-risk demographics in order to combat the rising prevalence of metabolic syndrome.
The present study has certain limitations. First, there may be some selection bias. Health conscious individuals with an inherent interest in wellness, or with a higher monthly household income may be more inclined to participate in our survey. Their knowledge about metabolic syndrome, and better access to health information due to their socioeconomic status might have influenced their responses, resulting in an overestimation of the overall awareness level in the general population. Therefore, the awareness of metabolic syndrome could be lower than that seen in our results. Second, the generalizability of our findings is limited because of the geographic scope of our study, which was restricted to Korean adults aged 20–69 years. Therefore, the results may not be applicable to other ethnicities or age groups. Third, the evaluation of metabolic syndrome awareness was based on subjective responses rather than on a standardized scoring system. This subjective approach might have limited accuracy in assessing the participants’ actual knowledge of metabolic syndrome. However, future studies might benefit from incorporating more objective measures to further validate self-reported awareness levels. Despite these potential limitations, our study aimed to bridge the gap between subjective self-perception and actual knowledge of metabolic syndrome in the Korean population. The results of awareness, as self-reported by the participants, can be considered meaningful in shedding light on this crucial public health issue.
Our study offers valuable insights into awareness of metabolic syndrome and its influencing factors in the Korean adult population. This study unveils a substantial gap in the awareness of metabolic syndrome among Korean adults, despite the varied demographic representation ensured by stratified systematic sampling. Our findings underscore the crucial role of awareness in recognizing the importance of lifestyle modifications and actively engaging in health-promoting behaviors. Furthermore, the identification of certain risk factors, including younger age, lower household income, and absence of comorbid conditions, contributes to the deficit in awareness and provides a roadmap for designing targeted interventions. As we move forward, it is imperative to deploy concerted efforts towards comprehensive educational strategies that are personalized according to these risk factors to bolster the understanding and management of metabolic syndrome. Such an approach will not only help individuals become active participants in their own health management, but also enable us to navigate towards a healthier society.
In conclusion, it is clear that our study highlights a significant awareness gap regarding metabolic syndrome among Korean adults, revealing that age, income, and absence of comorbid conditions can affect this awareness. These findings emphasize the need for personalized educational strategies, promotion of better self-management of health, and steering society towards improving overall health.
KEY MESSAGE
1. There was a significant gap in the awareness of metabolic syndrome among Korean adults.
2. The high-awareness group showed more knowledge of the importance of lifestyle modifications and better health behaviors regarding metabolic syndrome.
3. Certain risk factors, including younger age, lower household income, and absence of comorbid conditions, contribute to the deficit in awareness of metabolic syndrome.
4. The findings highlight the need for improved public education and awareness programs regarding metabolic syndrome.
Acknowledgments
The authors thank the Korean Society of CardioMetabolic Syndrome for providing the funds for this online survey.
Notes
CRedit authorship contributions
Hyun-Jin Kim: methodology, data curation, writing - original draft; Mi-Seung Shin: conceptualization, methodology, writing - review & editing, supervision, project administration; Kyung-Hee Kim: methodology; Mi-Hyang Jung: methodology; Dong-Hyuk Cho: methodology; Ju-Hee Lee: methodology; Kwang Kon Koh: writing - review & editing, supervision
Funding
None