Self-screening questionnaire for perianal fistulizing disease in patients with Crohn’s disease
Article information
Abstract
Background/Aims
A poor prognostic factor for Crohn’s disease (CD) includes perianal fistulizing disease, including perianal fistula and/or perianal abscess. Currently, a tool to assess perianal symptoms in patients with CD remains nonexistent. This study aimed to develop a perianal fistulizing disease self-screening questionnaire for patients with CD.
Methods
This prospective pilot study was conducted at three tertiary referral centers between January 2019 and May 2020. We formulated questions on perianal symptoms, including tenesmus, anal discharge, bleeding, pain, and heat. A 4-point Likert scale was used to rate each question. Patients with CD completed a questionnaire and underwent pelvic magnetic resonance imaging (MRI).
Results
Overall, 93 patients were enrolled, with 51 (54.8%) diagnosed with perianal fistulizing disease, as determined by pelvic MRI. The Spearman correlation findings demonstrated that anal pain (p = 0.450, p < 0.001) and anal discharge (p = 0.556, p < 0.001) were the symptoms that most significantly correlated with perianal disease. For anal pain and discharge, the area under the receiver operating characteristic curve of the scores was significantly higher than that of the combined score for all five symptoms (0.855 vs. 0.794, DeLong’s test p = 0.04). For the two symptoms combined, the sensitivity, specificity, and positive predictive and negative predictive values were 88.2, 73.8, 80.4, and 83.8%, respectively, with 81.7% accuracy for detecting perianal fistulizing disease.
Conclusions
This study indicates that simple questions regarding anal pain and discharge can help accurately identify the presence of perianal fistulizing disease in patients with CD.
INTRODUCTION
Crohn’s disease (CD) is described as a chronic inflammatory condition of the gastrointestinal tract with a relapsing and remitting clinical course. A peculiar CD phenotype is perianal fistulizing Chron's disease (pCD), such as perianal fistula and abscess. A recent nationwide cohort study reported that approximately 15–30% of CD patients develop pCD [1]. At least two-thirds of patients with CD undergo fistulotomy or percutaneous drainage procedures at some point in their lives [2]. In the incidence of perianal involvement, racial differences exist, in which it is higher among Asian (23%) and Black (31%) patients with CD than in Caucasians (14%) [3].
Furthermore, pCD is well known as a poor prognostic factor for CD. It is associated with increased symptom severity and the need for immunosuppressive treatment, hospitalization, and bowel resection, ultimately leading to an impaired quality of life [4,5]. Thus, early detection of pCD and robust disease activity monitoring are important in managing pCD in patients with CD.
Early detection of pCD enables the early use of appropriate antibiotics, thiopurines, and tumor necrosis factor (TNF)-α inhibitors, which possess strong evidence supporting their use in pCD treatment [6,7], and/or surgical drainage with seton insertion depending on whether the perianal fistula type is simple or complex [8,9]. Serious complications can be prevented through a timely and multidisciplinary approach such as anal stricture or total proctectomy with ileostomy [10,11].
Hence, it is vital for patients with CD to identify their pCD symptoms. However, no self-screening tool is available for pCD management. We aimed to develop a self-screening questionnaire that can promptly detect perianal fistula or abscess in patients with CD.
METHODS
Patients and study design
This pilot study, with a prospective cross-sectional design, was conducted at three tertiary referral centers between January 2019 and May 2020. Consecutive adult and pediatric patients diagnosed with CD were enrolled. The diagnosis of CD was based on symptoms, laboratory tests, endoscopic and radiological findings, and pathologic features [12,13]. The Montreal Classification of CD, based on disease location (L1 ileal, L2 colonic, and L3 ileocolonic) and behavior (B1 nonstricturing non-penetrating, B2 stricturing, B3 penetrating), was employed [14]. At enrollment, disease activity was assessed using the Harvey–Bradshaw index (HBI) [15], and laboratory tests including C-reactive protein (CRP) and white blood cell (WBC) count were performed. Patients completed a questionnaire for their perianal symptoms and underwent pelvic magnetic resonance imaging (MRI) within 2 weeks of the survey as the gold standard for determining the presence of a perianal fistula and/or abscess [16]. Informed consent was obtained from the patients and guardians. This study was approved by the Institutional Review Board of each participating hospital (Kyungpook National University Hospital, protocol code KNUH 2016-11-008) and conducted in compliance with the principles of the Declaration of Helsinki.
Questionnaire development for perianal symptoms
Five gastroenterologists (E.S.K., B.K., K.O.K., H.S.L., and B.I.J.) with greater than 10 years of experience in managing patients with CD devised questions regarding perianal symptoms after a literature review. Anal pain and discharge, rectal bleeding, swelling, and incontinence were confirmed as the major pCD symptoms [17,18]. They discussed and rated each symptom several times via E-mail to modify and select the final symptoms. Swelling was excluded as a variable as anal swelling or induration is more accurately evaluated by surgeons and not the patient. Incontinence was excluded because it tends to occur late or is related to surgically induced damage to the anal sphincter. Instead, tenesmus and “anal heat” sensation, which are more easily assessed by patients, were included. The five selected questions were on anal discharge, anal bleeding, anal pain, tenesmus, and anal heat (Fig. 1). For the questionnaire, each question was rated on a 4-point (0 to 3) Likert scale.
Statistical analysis
Categorical variables are expressed as numbers and proportions, and to compare clinical characteristics between the groups, Fisher’s exact test was used. Continuous variables are presented as mean ± standard deviation (SD) or median with interquartile range and were compared using student’s t-test or Mann–Whitney U test. The Spearman correlation coefficient was used to evaluate the correlation between perianal lesions and questionnaire items, CRP level, WBC count, and HBI. The optimal cutoff values of independent variables for differentiation between the total score and the presence of perianal disease were selected using receiver operating characteristic (ROC) curve analysis. Diagnostic accuracy was evaluated using the area under the curve (AUC), and AUCs between groups were compared using DeLong’s test. We analyzed the sensitivity, specificity, PPV, NPV, and accuracy for predicting pCD. Statistical significance was set at a p value < 0.05. Statistical analyses were conducted using SPSS software (version 19.0; IBM Corp., Armonk, NY, USA).
RESULTS
Baseline characteristics of the enrolled patients
Overall, 93 patients aged 9 to 64 years (mean age ± SD: 21.8 ± 8.5 years) were enrolled in this study. Table 1 demonstrates the baseline characteristics of the patients, in which the patients were divided by the presence of pCD according to findings on pelvic MRI. Most baseline variables were not significantly different between the two groups. The perianal lesion group had a relatively higher proportion of ileocolic locations than the group without perianal lesions (80.4% vs. 59.5%, p = 0.084), although with no statistical significance.
Comparison of clinical factors and patient symptoms based on the presence of perianal disease
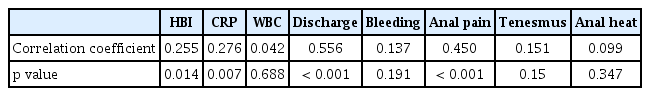
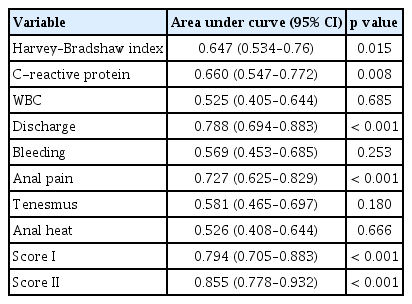
In the groups with and without pCD, the median HBI was 6 vs. 3 (p = 0.014), respectively, and the CRP level was 1.41 vs. 0.32 (p = 0.008). No significant difference was found between the groups in the WBC count. Regarding perianal symptoms, the pCD group revealed a significantly higher median score of anal discharge (1 vs. 0, p < 0.001) and pain (1 vs. 0, p < 0.001) than patients without pCD. No significant difference was found between the groups in the scores for bleeding, tenesmus, and anal heat (Table 2). The Spearman correlation coefficient (p) of anal discharge and anal pain were the highest at 0.556 (p < 0.001) and 0.45 (p < 0.001), respectively, suggesting a moderate level of correlation of anal discharge and pain symptoms with pCD. HBI (0.255, p = 0.014) and CRP (0.276, p = 0.007) were weakly correlated (Table 3) [19]. WBC count, bleeding, tenesmus, and anal heat exhibited no correlation with pCD.
Comparison of clinical factors and scores of each symptom between patients with or without perianal fistula
ROC analysis of clinical factors and the five questionnaire items
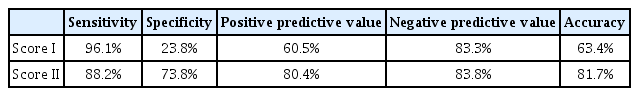
The AUCs of HBI, CRP, and WBC count were 0.647 (p = 0.015), 0.660 (p = 0.008), and 0.525 (p = 0.685), respectively (Table 4, Fig. 2A). The AUCs of anal discharge and anal pain were 0.788 (p < 0.001) and 0.727 (p < 0.001), respectively. This was higher than those of anal bleeding (0.569, p = 0.253), heat (0.526, p = 0.666), and tenesmus (0.581, p = 0.180) (Fig. 2B). Next, we calculated the composite scores for predicting pCD in patients with CD. Score I was the sum of all five questionnaire item scores, and Score II was the sum of anal discharge and pain scores. The AUC of Score II was significantly higher than that of Score I (0.855, p < 0.001 vs. 0.794, p < 0.001, DeLong’s test p = 0.04, Table 4, Fig. 2C).

ROC curve analysis of the clinical and laboratory results. (A) CRP level, HBI value, and WBC count, (B) the five questionnaire symptoms, and (C) the composite scores. Score I is the sum of the five questionnaire item scores. Score II is the sum of the anal discharge and anal pain scores. ROC, receiver operating characteristic; CRP, C-reactive protein; HBI, Harvey–Bradshaw index; WBC, white blood cell.
Efficacy of self-completed questionnaire for predicting perianal disease in patients with CD
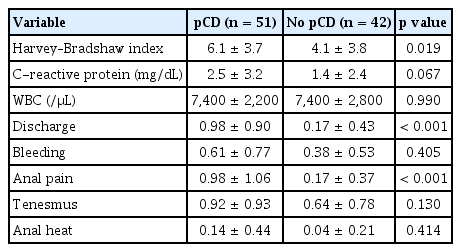
The performance of the composite questionnaire scores, Score I and Score II, for predicting pCD is illustrated in Table 5. According to the ROC curve, score 1 (among 0–3) was found to be the optimal cutoff value for the highest accuracy. The sensitivity, specificity, PPV, and NPV were 96.1, 23.8, 60.5, and 83.3%, respectively, for Score I and 88.2, 73.8, 80.4, and 83.8%, respectively, for Score II. Score II was more accurate than Score I (accuracy 81.7% vs. 63.4%, respectively, Table 5).
DISCUSSION
We developed a self-screening tool for pCD in patients with CD. The questionnaire constituted five simple questions regarding anal discharge, anal pain, bleeding, tenesmus, and anal heat. In a cross-sectional study, we found that anal discharge and pain had a moderate correlation with pCD, whereas other symptoms were not significantly correlated. The composite score of anal discharge and pain detected perianal disease with 81.7% accuracy.
One of the unmet needs in pCD management is the lack of a clinical index that can be easily utilized by patients. Given that pCD is more common in pediatric patients [20], a simple, child-friendly tool is warranted. In 1992, an anal disease activity index was developed for use in the outpatient clinic or at the patient’s bedside [21]. It evaluated seven symptoms or activities, including perianal pain, itching, pain during defecation, anal leakage, inhibition of locomotion, and social and sexual activity. Only pain-related symptoms such as perianal pain, pain after defecation, and inhibition of locomotion by pain demonstrated a high discriminative value as an index of response to therapy. However, this index was not developed to detect perianal fistulas. Furthermore, the sexual activity variable was not suitable for children. Other activity indices, such as the perianal disease activity index [22], fistula drainage assessment [6], and Pikarsky’s perianal activity index [23], assess disease severity and response to therapy and help predict outcomes. However, they are complex and have variables that need to be measured by the doctor and are not useful as a self-screening tool for pCD.
The first manifestation of CD in approximately 10% of patients is perianal fistula and/or abscess. It can occur several years prior to luminal CD onset [24]. Perianal disease activity does not always parallel luminal activity and may be present when the luminal disease is inactive in a subset of patients [25]. Hence, traditional clinical indices for evaluating luminal CD activity may not be appropriate for pCD activity. In this study, Spearman correlation and ROC analysis revealed that pCD was mostly associated with anal pain and discharge rather than with HBI, CRP, and WBC (Table 3, 4). Therefore, anal pain and discharge are more accurate variables for predicting the presence of perianal complications than indicators of luminal CD activity and biomarkers of systemic inflammation. We included CRP (cutoff 1.33 mg/dL) and HBI (cutoff score 4) in the Score model (anal pain, anal discharge, HBI, and CRP). The AUC of this model was 0.849 (0.774–0.924, p < 0.001, sensitivity 82.4%, specificity 73.8%, positive predictive value 79.2%, negative predictive value 77.5%), which was not greater than the AUC of Score II (anal pain and anal discharge).
Early detection of anorectal disease is pivotal for the decision making in CD management. pCD assessment using an easily administered screening tool in routine clinical practice may help detect patients who require pelvic MRI or anal ultrasonography and promote timely management of pCD. In patients with complex pCD, this approach with a screening tool may allow the prompt use of advanced therapies, such as mesenchymal stem cell local therapy [26,27] or TNF-α inhibitors, which can be effective in reducing the need for surgical treatment or in minimizing postoperative complications [6,28]. In the present study, the questionnaire can help detect pCD early and easily in outpatients, rendering it as an effective anorectal disease screening tool in CD. Moreover, 25 of the 93 study patients were under 18 years of age, an age at which early disease detection is important. We conducted a subgroup analysis in the adult vs. children’s group according to age. The AUC (95% confidence interval) of Score II in the children group (0.792, 0.599–0.984, p = 0.132) appeared to be lower than the AUC in the adult group (0.851, 0.768–0.934, p = 0.009). However, caution must be exercised in interpreting data as the small sample size in the children group might have affected the performance of the Score II model.
One might argue that the perianal fistula in CD should be evaluated by colorectal surgeons. However, gastroenterologists can initially assess the status of patients and refer them to surgeons with suspicion of perianal symptoms. Thus, gastroenterologists and even patients themselves need to understand the typical symptoms of perianal disease in CD patients to be timely sent to and further evaluated by surgeons. There has been no study to estimate perianal symptoms from the patients’ or gastroenterologists’ perspectives. We believe that the study results might aid gastroenterologists screen the appropriate patients for further evaluation of pCD by surgeons or MRI.
This study has limitations. This study was designed as a pilot study, and the sample size was small. However, statistically significant differences were observed among variables in detecting pCD. Furthermore, because this was a cross-sectional study, the study results were not validated in an independent cohort, and the effectiveness of this tool for measuring response to therapy remains unclear. We acknowledge that anal pain and discharge are among the already known symptoms of pCD. However, there is paucity of research on the extent to which these symptoms are associated with concurrent perianal disorders. In a future longitudinal study, assessment of the prognosis of screened patients with perianal complications who are promptly referred to colorectal surgeons is warranted to validate the efficacy of the screening tool.
In conclusion, this study identified anal discharge and pain as the most effective predictive factors for pCD among various anal symptoms. The self-screening questionnaire on anal discharge and pain is an effective and a valuable tool for detecting pCD in children and adults with CD. This screening tool’s performance should be confirmed in an independent cohort, and its efficacy for monitoring patients with pCD should be evaluated in further longitudinal studies.
KEY MESSAGE
1. Simple questions regarding anal pain and discharge can help accurately identify the presence of perianal fistulizing disease in patients with CD.
2. A simple questionnaire regarding anal pain and discharge, which can be easily filled in by patients at outpatient clinics, can be used as an effective screening tool for detecting perianal fistula or abscess in children and adult patients with CD.
Notes
CRedit authorship contributions
O Seong Kweon: methodology, resources, investigation, data curation, formal analysis, software, writing - original draft, writing - review & editing; Ben Kang: resources, data curation; Yoo Jin Lee: resources, data curation; Eun Soo Kim: conceptualization, methodology, resources, investigation, data curation, formal analysis, validation, writing - review & editing, visualization, supervision, project administration, funding acquisition; Sung Kook Kim: resources, data curation; Hyun Seok Lee: resources, data curation; Yun Jin Chung: resources, data curation; Kyeong Ok Kim: resources, data curation; Byung Ik Jang: resources, data curation
Conflicts of interest
The authors disclose no conflicts.
Funding
This work was supported by a Biomedical Research Institute grant of Kyungpook National University Hospital (2021).
Data availability statement
The data underlying this article will be shared on reasonable request to the corresponding author.