A patient with dyspnea and multiple pulmonary nodules
Article information
A 62-year-old male with a 30-pack-year smoking habit was admitted to our clinic with dyspnea. A chest computed tomography (CT) scan revealed a spiculated mass with enhancement in the left upper lobe (LUL; Fig. 1A) and concurrent multiple pulmonary nodules (Fig. 1B). 2-Deoxy-2-[18F]-fluorodeoxyglucose (FDG) positron emission tomography (PET)/CT demonstrated FDG avidity in LUL nodule (Fig. 1C).
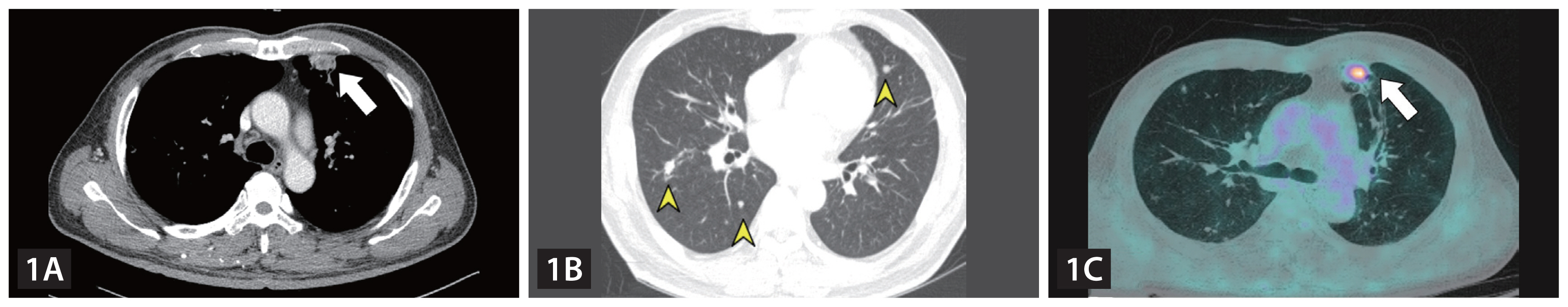
(A) A chest computed tomography (CT) scan revealed a 2.1 × 1.7 × 1.3 cm spiculated mass with enhancement in the left upper lobe of lung, anterior segment of subpleura (arrow). (B) A chest CT scan revealed diffused round multiple pulmonary nodules (arrow heads). (C) 2-Deoxy-2-[18F]-fluorodeoxyglucose (FDG) positron emission tomography (PET)/CT revealed 2 cm FDG-avid nodular region in the left upper lobe anterior subpleural portion (SUVmax = 3.70, arrow).
The patient underwent thoracoscopic wedge resection of LUL nodule and histopathology revealed a chronic granulomatous inflammation associated with several yellow-brown and ovoid eggs with a thick shell, all of which were characteristic attributes of pulmonary Paragonimus westermani infection (Fig. 2A). The patient did not reveal any special diet containing raw or undercooked fish. Blood P. westermani antibodies were positive and serum total Ig-E level was elevated up to 1,663.1 UI/mL. Based on these findings, the patient was treated with praziquantel. At the same time, 1.9 cm FDG-avid lesion in left submandibular gland was detected during the work-up. However, further evaluation on the lesion was impossible owing to patient’s refusal.

(A) The subsequent wedge resection of the same left upper lobe nodule in both Figure 1A and 1C showed a chronic granulomatous inflammation associated with several yellow-brown, ovoid eggs with a thick shell, all of which are characteristic features of pulmonary Paragonimus westermani infection. Bar indicates scale of 200 μm (H&E stain, × 50). (B) In a follow-up chest computed tomography (CT), remnant pulmonary nodules presented as larger than before with solitary change (arrow heads). (C) In a follow-up 2-Deoxy-2-[18F]-fluorodeoxyglucose (FDG) positron emission tomography (PET)/CT, some nodules increased in size and metabolism compared with previous FDG-PET/CT (arrow). (D) Wedge resection of two remaining nodules in the superior lingular segment exhibiting growth characteristics revealed it was poorly differentiated metastatic carcinoma which had hyperchromatic and pleomorphic nuclei. Bar indicates scale of 100 μm (H&E stain, × 200). (E) Initial PET/CT scan demonstrated increased FDG avidity in the left submandibular gland, suggesting the presence of primary malignancy in this area (SUVmax = 5.02). (F) The excisional biopsy of the submandibular gland revealed carcinoma ex pleomorphic adenoma appearing as pleomorphic tumor cell infiltrating into the benign adenoma. Bar indicates scale of 100 μm (H&E stain, × 50). The histopathological similarity of the resected lung mass and left submandibular gland confirmed metastatic lung cancer from carcinoma ex pleomorphic adenoma.
Five months after treatment, follow-up high-resolution computed tomography (HRCT) images showed increased size of remnant pulmonary nodules (Fig. 2B) and in follow-up FDG-PET/CT scan, some nodules had augmented metabolism (Fig. 2C). Wedge resection of remaining FDG-avid nodules in the superior lingular segment revealed that it was poorly differentiated metastatic carcinoma which had a hyperchromatic and pleomorphic nuclei (Fig. 2D). Results from PET/CT scans demonstrated increased FDG avidity in the submandibular gland, suggesting presence of primary malignancy in this area (Fig. 2E). Finally, excisional biopsy of the submandibular gland confirmed carcinoma ex pleomorphic adenoma which appeared as pleomorphic tumor cell infiltrating into the benign adenoma (Fig. 2F).
Herein, we demonstrated an extremely rare case of metastatic lung cancer originating from salivary gland concurrent with parasitic lung infection. Even though paragonimiasis has been frequently reported to mimic primary lung cancer [1–3], the possibility for the coexistence of paragonimiasis with malignant lung lesion from various origins should not be overlooked in clinical practice.
Notes
CRedit authorship contributions
Jae Seok Jeong: investigation, validation, writing - review & editing; Jun Hyung Park: writing - original draft; Ji In Maeng: writing - original draft; Myoung Ja Chung: resources, investigation, validation; Yong Chul Lee: resources, validation, writing - review & editing
Conflicts of interest
The authors disclose no conflicts.
Funding
This research was supported by the Bio&Medical Technology Development Program of the National Research Foundation (NRF) funded by the Korean government (MSIT) (No. RS-2023-00236157). This paper was supported by Fund of Biomedical Research Institute, Jeonbuk National University Hospital and research funds for newly appointed professors of Jeonbuk National University in 2023.
