Initial and Late Results of Freedom Coronary Stent
Article information
Abstract
Objectives
Initial and late results after implantation of Freedom stents, a balloon expandable stainless steel coil stents were evaluated.
Methods
From Jun. 1996 to Nov. 1997, we implanted 123 Freedom stents in 122 lesions in 117 patients and performed follow-up coronary angiograms at 7.0 ± 3.6 months after stents placement. Clinical courses after stenting and follow-up coronary angiographic findings were evaluated. Comparison of clinical, angiographic, and procedural factors according to the presence or absence of restenosis was performed.
Results
In 117 patients who underwent stents implantation, major complications were not observed. Follow-up coronary angiograms were performed in 47 stents in 41 patients (35%). Among 47 stents, angiographic significant restenosis (percent diameter stenosis > 50%) was observed in 13 (28%). Mean age in 41 patients was 59 ± 9 years, with 27 male patients (66%). Indications for stents implantation were de novo lesions in 18 (38%), suboptimal results after PTCA in 18 (38%), bail-out lesions in 4 (9%) and restenotic lesions in 7 (15%). Lesion types by AHA/ACC classification were A in 1 (1%), B1 in 10 (21%), B2 in 17 (36%), and C in 19 (40%). Average lesion length was 13.7 ± 9.0mm, stent diameter 3.0 ± 0.3mm, and stent length 24.6 ± 9.0 mm. There were no significant differences of the clinical, angiographic, and procedural characteristics according to the presence or absence of restenosis.
Conclusion
Freedom coronary stents implantation is safely performed in various morphology of coronary lesions and no significant predictive factors on restenosis in follow-up coronary angiogram were observed.
INTRODUCTION
Percutaneous transluminal coronary angioplasty (PTCA) is now an established treatment for patients with coronary artery disease since first introduced by Andreas Gruentzig in 1977. Though improvements in techniques and devices permit a high primary success rate, acute or threatened closure and frequent restenosis of the dilated segments are major obstacles to expanding its usefulness and limit the long-term benefit in patients who underwent successful coronary angioplasty1–4).
Although a lot of pharmacological and mechanical intervention has been attempted to prevent restenosis after PTCA, stents have evolved as a reliable technique for treating arterial dissection and impending vessel closure and a beneficial effect on late restenosis5–7). Considerable experience has been gained with Palmaz-Schatz stent, Wallstent, Gianturco-Roubin stent, Wiktor stent, Microstent, NIR stent, and Cordis stent etc8–15).
Freedom coronary stent has been developed by Global Therapeutics and clinically available. Major advantages of Freedom coronary stents are 1) a low profile (6 Fr. compatible) flexible coil stent, showing sufficient trackability even when using the long versions (36–40 mm), 2) variable stent lengths (up to 40 mm) promoting the single balloon/single stent principle-cost saving and reduce overlapping stents, 3) superior conformability to vessel contour, 4) good radio-opacity, and 5) good for bifurcation (Figure 1).
In this paper, we report the initial clinical outcome and long-term predictive factor for stent retenosis after placement of Freedom coronary stents.
PATIENTS AND METHODS
1. Device description
The Freedom coronary stent is constructed of 316LVM stainless steel wire with a cross-sectional diameter of 0.175 mm. Profile before delivery was 1.30 mm and surface area after expansion was 11%. Lengths available were 12, 16, 20, 24, 30, and 40 mm and diameters available were 2.5, 3.0, 3.5, 4.0, and 4.5 mm. The stents were balloon-expandable and premounted on a balloon without a sheath.
2. Stent procedure
From Jun. 1996 to Nov. 1997, 117 patients with 122 lesions underwent the implantation of Freedom coronary stents for de novo lesions, suboptimal results after PTCA, bailout lesions, and restenotic lesions. Five had multiple stents (2 stents in 4 patients and 3 stents in 1 patient) and 112 patients had a single stent in their native coronary artery. Freedom coronary stents were placed into the coronary arteries following the predilation of the stenotic lesions by the standard balloon angioplasty. The stents were inserted into into coronary artery by over-the-wire technique under fluoroscopic guidance and were planted in the vessel wall by balloon inflation at maximal balloon pressure of 11 ± 2mmHg, then the balloons were withdrawn from the lesion after deflation. During the study, high-pressure inflations, oversized balloons, and intravascular ultrasound were not routinely used. Patients were premedicated with aspirin and ticlopidine. During the procedure, heparin (10,000 units) was administered. After stents implantation, all patients received aspirin (100 mg twice a day) continuously and ticlopidine (250 mg twice a day) for four weeks.
3. Follow-up coronary angiogram
Follow-up coronary angiogram was performed at 7.0 ± 3.6 months after Freedom coronary stent placement in patients with myocardial ischemia or infarction. Measurements were performed by the electronic hand caliper. Calibration was done by the guiding catheter. Restenosis was defined as more than 50% diameter stenosis. Comparison of clinical, angiographic, and procedural factors according to the presence or absence of restenosis was performed.
4. Statistical analysis
All data are expressed as the mean value ± SD. Comparisons were performed using t-tests for continuous variables and the chi-square tests for dichotomous variables. A statistical probability of p ≤ 0. 05 was considered significant.
RESULTS
1. Studied Subjects
In 117 patients who underwent the stents implantation, the major complications, including death, emergency bypass surgery, major bleeding transfusion or Q wave myocardial infarction, were not observed. Acute myocardial infarction was present in 53 patients (45%), unstable angina in 50 (43%), and stable angina in 14 (12%). Follow-up coronary angiograms (7.0 ± 3.6 months) were performed in 41 patients (35%).
In 41 patients who underwent follow-up coronary angiograms, mean age was 58.5 ± 8.7 years, with 27 male patients (66%). Among 47 stents in 41 patients, acute myocardial infarction was present in 21 (45%), unstable angina in 20 (43%), and stable angina in 6 (12%). Risk factors were diabetes mellitus in 13 (28%), hypertension in 23 (49%), hyperlipidemia (total cholesterol 2≥240 mg/dl) in 20 (43%), and smoking in 31 (66%). Left ventricular ejection fraction < 40% was in 4 (9%). Stent indications were de novo lesions in 18 (38%), suboptimal results after PTCA in 18 (38%), bail-out lesions in 4 (9%), and restenotic lesions in 7 (15%). Single vessel disease was present in 22 (47%), double vessel disease in 18 (38%), and triple vessel disease in 7 (15%). The stented arteries were the left anterior descending artery in 31 (66%), the circumflex artery in 7 (15%), and the right coronary artery in 9 (19%). Lesion types by AHA/ACC classification were A in 1 (2%), B1 in 10 (21%), B2 in 17 (36%) and C in 19 (41%). Average lesion length was 13.7 ± 9.0mm, stent diameter 3.0 ± 0.3 mm, and stent length 24.6 ± 9.0mm.
2. Follow-up coronary angiogram
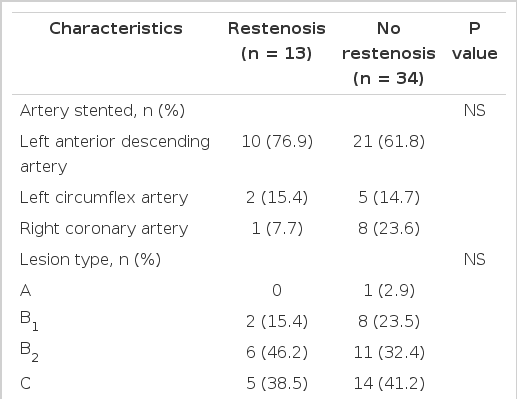
Among 47 stents in 41 patients, angiographic significant restenosis (percent diameter stenosis > 50%) was observed in 13 patients (28%). There were no significant differences of the clinical, angiographic, and procedural characteristics between restenosis and no restenosis groups (Table 1–3).
DISCUSSION
Our clinical experiences of Freedom coronary stents were reported. We easily and safely implanted the stent even in long, angulated lesions. During and just after stent implantation, no major complications such as death, emergent bypass surgery, and Q wave myocardial infarction were developed.
Restenosis rate of the stent was reduced by about 22–31% compared to balloon angioplasty. The restenosis rate of Freedom coronary stents in our experience was 28%. It is not a true restenosis rate because all of the patients who had implanted Freedom stents did not undergo follow-up coronary angiogram. And we preferred to implant Freedom stents at long, angulated lesions because it remained flexible and trackable even at those lesions. Previously, we reported the early outcome of long coronary stents16).
The major mechanisms for chronic restenosis following angioplasty have been known, such as elastic recoil, intimal hyperplasia, thrombus, and arterial remodeling17–21). Many reports showed the fact that the stent could prevent elastic recoil and stent diameter did not change 6 months after the implantation suggested the restenosis following stenting might be due to thrombosis and intimal hyperplasia22).
Multiple trials using lipid lowering drugs, antimitotics, and other antiproliferative agents have failed to reduce intimal hyperplasia.
In our antithrombotic regimen, aspirin and ticlopidine were used for anti-platelet therapy. Recently, antagonists for glycoprotein IIb/IIIa receptors on the platelets have been introduced as effective antiplatelet agents to prevent restenosis after angioplasty.
In conclusion, Freedom coronary stents implantation is safely performed in the various morphology of coronary lesions and no significant predictive factors on restenosis in follow-up coronary angiograms were observedd.