Sex differences in long-term clinical outcomes of acute myocardial infarction according to the presence of diabetes mellitus
Article information
Abstract
Background/Aims
This study compared long-term clinical outcomes between male and female acute myocardial infarction (AMI) patients with and without diabetes mellitus (DM).
Methods
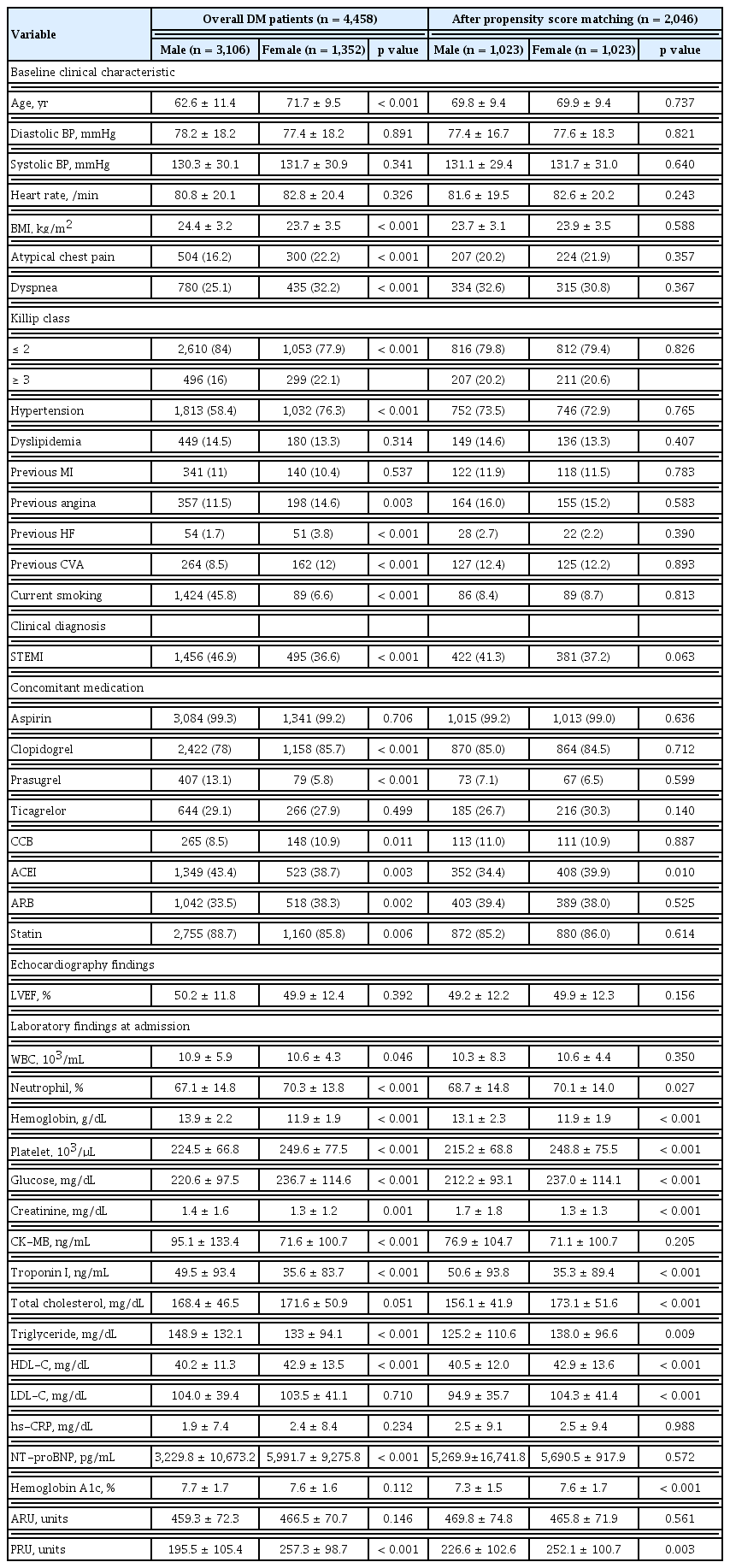
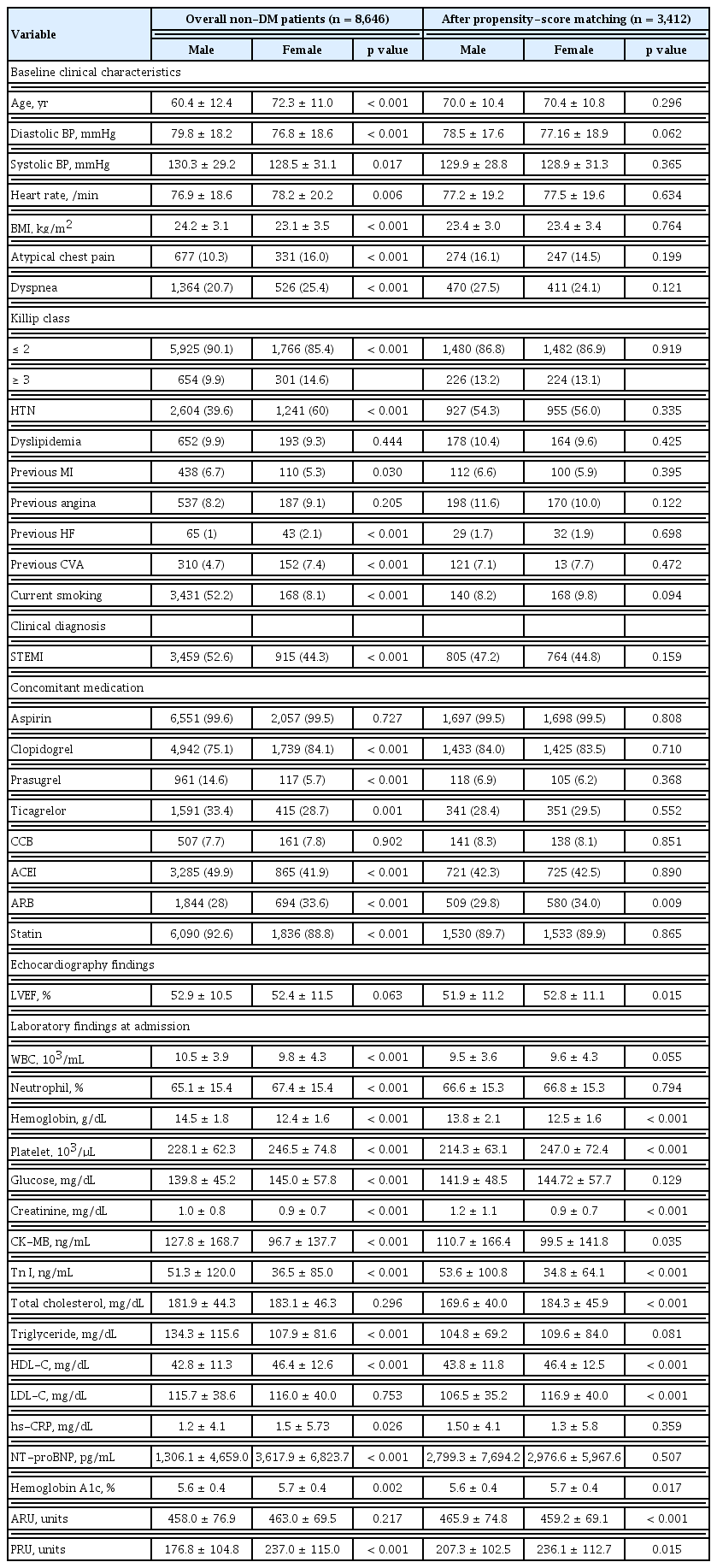
From November 2011 to December 2015, 13,104 patients with AMI were enrolled in the Korea Acute Myocardial Infarction Registry National Institutes of Health (KAMIR-NIH) (4,458 diabetic patients and 8,646 non-diabetic patients). Propensity score matching (PSM) was used to reduce bias due to confounding variables. Following PSM, 2,046 diabetic patients, 1,023 males (69.8 ± 9.4 years) and 1,023 females (69.9 ± 9.4 years); and 3,412 non-diabetic patients, 1,706 males (70.0 ± 10.4 years) and 1,706 females (70.4 ± 10.8 years) were analyzed. Clinical outcomes were compared between male and female patients with and without diabetes over a 3-year clinical follow-up.
Results
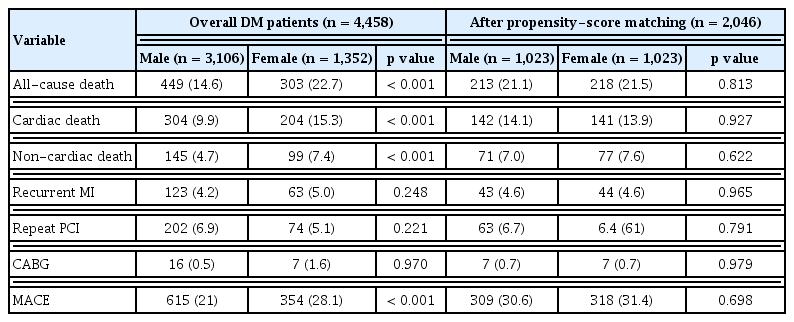
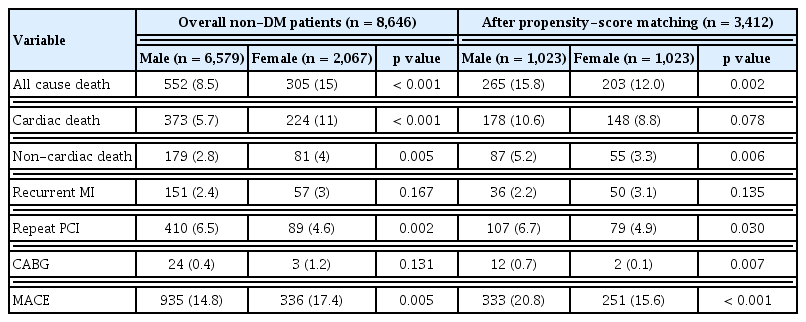
In diabetic patients, mortality (21.1% vs. 21.5%, p = 0.813) and major adverse cardiac events (MACE) (30.6% vs. 31.4%, p = 0.698) were not significantly different between males and females. However, mortality (15.8% vs. 12.0%, p = 0.002) and MACE (20.8% vs. 15.6%, p < 0.001) were significantly higher in male non-diabetic patients than in female non-diabetic patients. The predictors of mortality for both males and females in the diabetic and non-diabetic groups were old age, heart failure, renal dysfunction, anemia, and no percutaneous coronary intervention.
Conclusions
The long-term clinical outcomes in AMI patients with DM did not significantly differ by sex. However, the mortality and MACE in non-diabetic male patients were higher than those in females.
INTRODUCTION
The incidence of disease in Korea has shifted from acute to chronic diseases due to the development of the national economy, improvements in residential environment and nutritional status, and improvement in treatments. Mortality due to cardiovascular disease is steadily increasing, and in 2017, the number of deaths due to cardiovascular disease in Korea was 53,597 per year, accounting for approximately 19% of all deaths [1]. In particular, mortality due to heart disease has continued to increase over the past decade. Diabetes mellitus (DM) is a common chronic disease in Korea’s middle-aged population due to changes in diet and lifestyle. In the 2016 National Health and Nutrition Survey, the prevalence of diabetes in their 40s and 50s was 8.7% and 16.0%, respectively. It can be seen that the diabetes awareness rate over the age of 30 is 73.2%, and in particular, the control rate is 26.8%, which is very low. Therefore, screening the high-risk group for diabetes is an important issue in public health [2].
DM is a major risk factor for cardiovascular disease [3–5]. In addition, a study on the registration of acute myocardial infarction (AMI) in the United States showed that approximately 40% of AMI patients also have DM [6], while in Koreans, up to 41.8% of AMI patients have DM [7]. Mortality due to heart disease and stroke in diabetic patients is two to four times higher than that in non-diabetic patients, while previous studies have also found that mortality in diabetic patients with AMI is higher than that in non-diabetic patients with AMI [8–10].
The Atherosclerosis Risk in Communities (ARIC) studies of large numbers of people resulted in a total of 4.6% cardiac death or AMI [11]. The incidence of cases varied depending on the presence of DM and the history of AMI: 3.9% had no DM and no history of AMI, 10.8% had DM but no history of AMI, 18.9% had a history of AMI without DM, and 32.2% had DM and a history of AMI. The relationship between DM and AMI also differs by sex. When diabetic patients with coronary artery disease in Finland were compared by sex, the mortality rate due to cardiovascular disease higher in males than in females [12]. In contrast, in other study, the risk of major clinical events was higher in females than in males [13]. In Europe, the short-term prognosis of AMI patients with diabetes did not differ significantly by sex, but the long-term prognosis was different between males and females [14].
However, few studies have investigated sex-based differences in the long-term outcomes of diabetic patients with AMI in Korea [15], and thus, a long-term observational study is necessary. Therefore, this study aimed to compare the clinical characteristics of diabetic and non-diabetic patients with AMI by sex, registered in the Korea Acute Myocardial Infarction Registry-National Institutes of Health (KAMIR-NIH), and to identify the factors affecting major complications. In addition, this study aimed to provide important data for the treatment and management of diabetic and non-diabetic patients with AMI by examining the long-term clinical follow-up data over 3 years.
METHODS
Study design and population
This study was approved by the Institutional Review Board of Chonnam National University Hospital (CNUH-2020-132). The KAMIR-NIH study was also approved by the Institutional Review Board of Chonnam National University Hospital (CNUH 05-49), and was performed after obtaining consents from all subjects. The study was sponsored by the National Institute of Health as a prospective, multicenter, observational, and web-based cohort study for the development of prognosis and management indicators for patients with AMI, and the patients were registered at 20 major centers in Korea from November 2011 to December 2015.
The 13,104 AMI patients enrolled in KAMIR-NIH were as follows. The diabetic group comprised 4,458 patients, of which 3,106 (62.6 ± 11.4 years) were male, and 1,352 (71.7 ± 9.5 years) were female. The non-diabetic group comprised 8,646 patients, of which 6,579 (60.4 ± 12.4 years) were male, and 2,067 (72.3 ± 11.0 years) were female. Propensity score matching (PSM) was used to reduce bias due to variables. After PSM, of the 2,146 diabetic patients, 1,023 (69.8 ± 9.4 years) were male, and 1,023 (69.9 ± 9.4 years) were female. In the 3,412 non-diabetic patients, 1,706 (70.0 ± 10.4 years) were male, and 1,706 (70.4 ± 10.8 years) were female.
Definition and clinical endpoint
Information on general characteristics, including age, body mass index (BMI), Killip class, history, and smoking rate were collected. The clinical characteristics were recorded following hematological tests and echocardiographic examinations conducted during hospitalization to measure the left ventricular injection fraction (LVEF), while the lesion characteristics in coronary artery angiographic findings were classified using the American College of Cardiology/American Heart Association (ACC/AHA) classification [16]. The perfusion rate through coronary artery lesion was classified as thrombolysis in myocardial infarction (TIMI) flow [17].
Major adverse cardiac events (MACE) were defined as all cause death, recurrent myocardial infarction (MI), repeated percutaneous coronary intervention (PCI), and coronary artery bypass graft (CABG) during 3 years of clinical follow-up.
Statistical analysis
Continuous variables are presented as mean ± standard deviation and were compared using the Student’s t test. Discrete variables are expressed as percentages and frequencies and were compared by chi-square test. PSM analysis was performed using a multiple logistic regression model to minimize the selection bias when comparing the effect of sex. The relevant variables were included age, Killip class, hypertension, dyslipidemia, MI, angina, heart failure, cerebrovascular accident, BMI, smoking, pre-PCI, and post-PCI TIMI flow. The propensity score was calculated using logistic regression and matched one-to-one according to the propensity score value. C-statistic for the propensity score was 0.673. Multiple logistic regression and Cox proportional regression analyses were conducted to identify the independent predictors of 3-year mortality. The results are presented as adjusted hazard ratios with 95% confidence intervals. Kaplan–Meier curves were compared for all cause death and MACE, and the log rank test was used to test the differences in the survival curves.
All analyses were performed using SPSS software version 25.0 (IBM Co., Armonk, NY, USA). All analyses were two-tailed, and p values ≤ 0.05 were considered to be statistically significant.
RESULTS
Baseline characteristics and medication
The age of the female diabetic patients was significantly older than that of the male diabetic patients (62.6 ± 11.4 years vs. 71.7 ± 9.5 years, p < 0.001). The BMI was significantly higher in males than in females, and atypical chest pain and dyspnea were more frequently experienced in females than males. At admission, the Killip class was lower in males than in females. With respect to medical history, hypertension, previous angina, heart failure, and cerebrovascular events were significantly more frequent in females than males; however, smoking rates and incidence of ST segment elevation myocardial infarction (STEMI) were higher in males than in females. The use of clopidogrel, calcium channel blockers (CCB), and angiotensin-reflector blockers (ARB) was significantly lower in males, while the use of prasugrel, angiotensin-converting enzyme inhibitors (ACEI), and statins (p = 0.006) was significantly higher in males than females.
After PSM, the age of the diabetic patients (69.8 ± 9.4 years vs. 69.9 ± 9.4 years, p = 0.737) was not significantly different between males and females. The BMI, Killip class, hypertension, dyslipidemia, previous MI and angina, heart failure, cerebrovascular events, and smoking rates were not significantly different between males and females. The use of aspirin, clopidogrel, prasugrel, ticagrelor, CCB, ARB, and statin at hospitalization were also not significantly different between males and females (Table 1).
The age of the non-diabetic patients was significantly older in females than in males (60.4 ± 12.3 vs. 72.2 ± 11.0, p < 0.001). Systolic blood and diastolic blood pressures were higher in males, while the heart rate was higher in females. BMI was significantly higher in males than in females, and atypical chest pain and dyspnea were more frequently observed in females than in males. At admission, high Killip class, a history of hypertension, heart failure, and cerebrovascular events were more frequently noted in females than in males. Previous MI and smoking rates were significantly higher in males than in females, and STEMI was also more common in male. The use of clopidogrel and ARB was significantly lower in males than in females, while the use of prasugrel, ticagrelor, ACEI, and statin was significantly higher in males than in females.
After PSM, the age of the non-diabetic patients (70.0 ± 10.4 years vs. 70.4 ± 10.8 years, p = 0.296) was not significantly different between males and females. There were no significant differences in BMI, Killip class, hypertension, dyslipidemia, previous MI and angina pectoris, heart failure, cerebrovascular events and smoking rates. Use of aspirin, clopidogrel, prasugrel, ticagrelor, CCB, ACEI, and statin was not significantly different between males and females at hospitalization, although ARB were administered significantly more often in females than in males (Table 2).
Echocardiographic and laboratory findings
In the diabetic group, white blood cell (WBC) and lymphocyte counts and hemoglobin, creatinine, triglyceride, low-density lipoprotein cholesterol (LDL-C), creatine kinase-myocardial band (CK-MB), and troponin I levels were higher in males than in females. Neutrophil and platelet counts, platelet reactivity units (PRU), and high-density lipoprotein cholesterol (HDL-C), brain natriuretic peptide, N-terminal pro-brain natriuretic peptide (NT-proBNP), and glucose levels were significantly lower in males than in females. Although hemoglobin A1C (HbA1c) was found at relatively high levels, there was no significant difference between males and females. On echocardiography, there was no significant difference in the LVEF between males and females.
After PSM, in the diabetic group, hemoglobin, creatinine, and troponin I levels were significantly higher in males than in females, while the neutrophil, platelet count and glucose, total cholesterol, triglyceride, HDL-C, LDL-C, HbA1c, and PRU levels were significantly lower in males than in females (Table 1).
In the non-diabetic group, WBC and lymphocyte counts and hemoglobin, creatinine, CK-MB, troponin I, triglyceride, and high sensitivity C-reactive protein levels were higher in males than in females. Neutrophil and platelet counts and HDL-C, NT-proBNP, glucose, HbA1c, and PRU levels were lower in males than in females. On echocardiography, there was no significant difference in LVEF between males and females.
After PSM, in the non-diabetic group, hemoglobin, creatinine, CK-MB, ARU, and troponin I levels were significantly higher in males than in females, while the platelet counts, total cholesterol, HDL-C, LDL-C, PRU, and HbA1c levels were significantly lower in males than in females. The glucose level was not significantly different between males and females. LVEF was significantly lower in males than in females (Table 2).
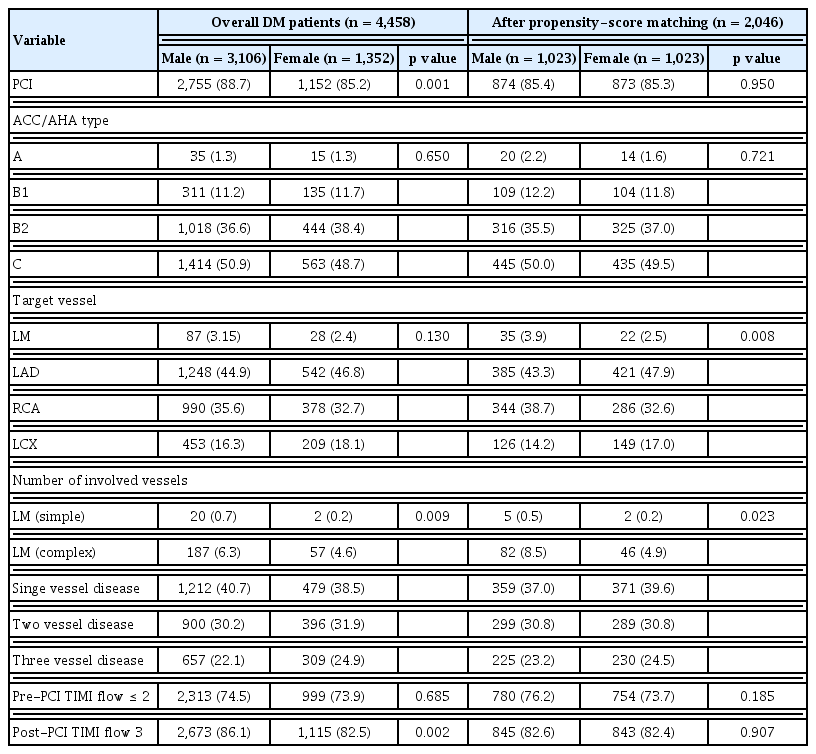
Coronary angiographic findings
In the diabetic group, PCI was more frequently performed in males than in females. Left main artery involved lesion and post-PCI TIMI flow 3 were significant higher males than females.
After PSM, in the diabetic group, there were no significant differences in lesion characteristics by the ACC/AHA classification and culprit lesion location. The culprit lesions of left main coronary artery was significantly higher in males (Table 3).
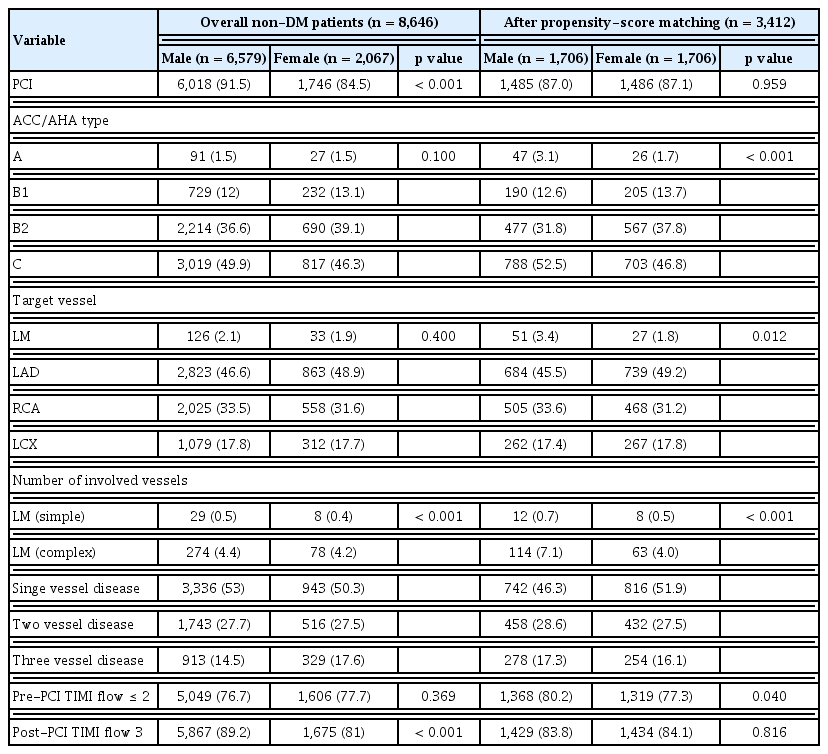
In the non-diabetic group, PCI was more frequently performed in males than in females. There were no significant differences in culprit lesions location and lesion characteristics by the ACC/AHA classification in both males and females. The TIMI III flow was higher in males than female after the procedure.
After PSM, in the non-diabetic group, the ACC/AHA lesion characteristics were significantly different between males and females, with more frequent C types in males. The culprit lesions of left main was significantly higher in males than females (Table 4).
Three-year clinical outcomes
In the diabetic group, over all the 3-year clinical follow-up, all cause death (p < 0.001), cardiac death (p < 0.001), non-cardiac death (p < 0.001), and MACE (p < 0.001) were significantly higher in females than in the males.
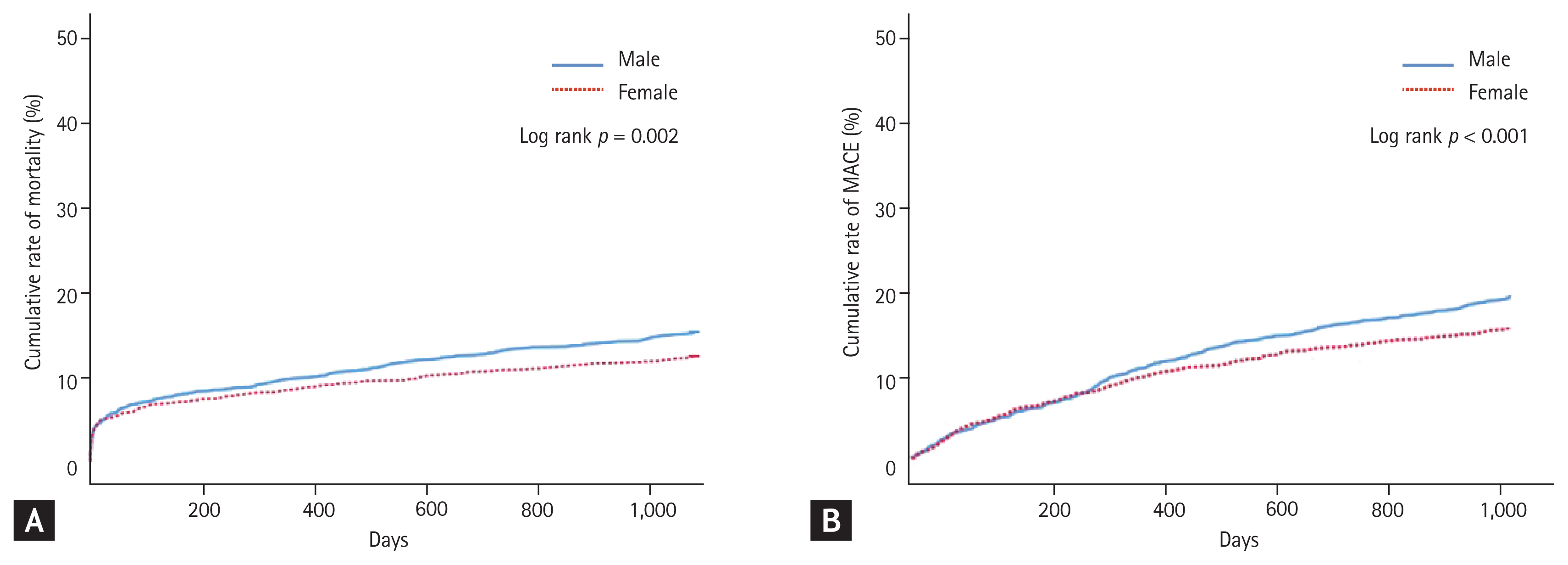
After PSM, in the diabetic group, the all cause death (p = 0.813) and MACE (p = 0.698) were not significantly different between males and females (Table 5). Analysis using Kaplan–Meier survival curves showed no significant difference between mortality and MACE in males and females in the diabetic group (Fig. 1).
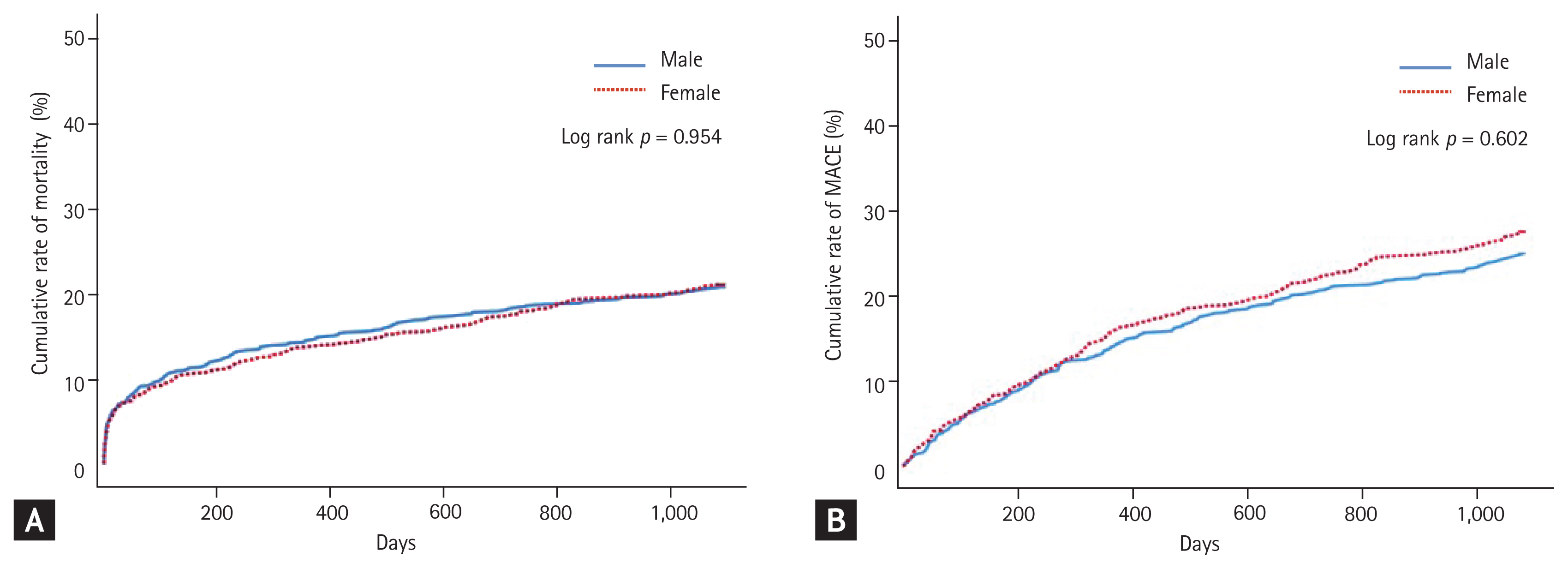
Kaplan–Meier curve for major adverse cardiac events (MACE) and mortality in diabetic patients with acute myocardial infarction. Cumulative rate of mortality (A) and MACE (B).
In the non-diabetic group, during 3-year follow-up, all cause death (p < 0.001), cardiac death (p < 0.001), non-cardiac death (p = 0.005), MACE (p < 0.001), and repeat PCI (p = 0.002) were significantly higher in females than in males.
After PSM, in the non-diabetic group, all cause death (p = 0.002), non-cardiac death (p = 0.006), MACE (p < 0.001), repeat PCI (p = 0.03), CABG (p = 0.007) were significantly higher in males than in females (Table 6). Analysis using Kaplan–Meier survival curves showed that mortality and MACE in the non-diabetic group were significantly higher in males than in females (Fig. 2).
Predictive factors of 3-year mortality
Predictors of mortality in males in the PSM diabetic group were old age over 65 years, low LVEF (< 40%), tachycardia (> 100, beats/min), high Killip class, high creatinine level (> 1.3 mg/dL), low hemoglobin level (< 12 g/dL) and no PCI, whereas in females, predictors included age over 65 years, low LVEF (< 40%), high creatinine level (> 1.3 mg/dL), low hemoglobin level (< 12 g/L), and no PCI (Table 7).
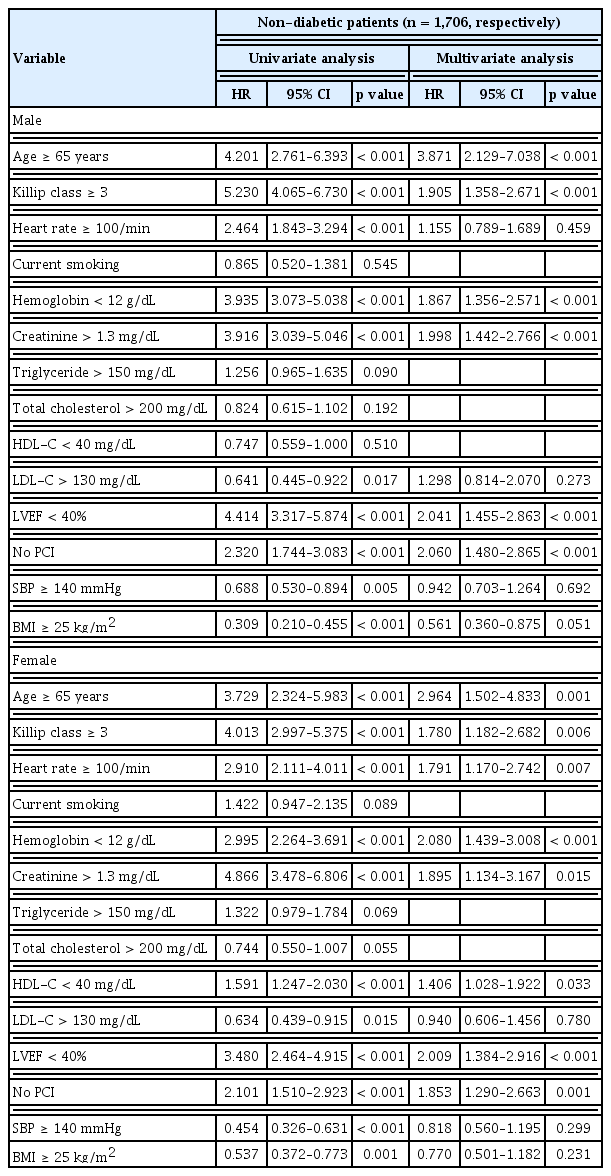
Predictors of mortality of males in the PSM non-diabetic group were age over 65 years, no PCI, low LVEF (< 40%), high creatinine level (> 1.3 mg/dL), high Killip class, and low hemoglobin level (< 12 g/dL), whereas in females, they were age over 65 years, low hemoglobin level (< 12 g/dL), low LVEF (< 40%), high creatinine level (> 1.3 mg/dL), tachycardia (> 100, beats/min), high Killip class, low HDL-C level ( > 40 mg/dL), and no PCI (Table 8).
DISCUSSION
In the PSM analysis, male and female AMI patients with DM were comparable in mortality, but male MI patients without DM had higher mortality rate and incidence of MACE than female AMI patients without DM.
According to the 2018 National Statistical Office data [18], the mortality rate of circulatory system disease was 122.7 per 100,000 populations, followed by heart disease, cerebrovascular disease, and hypertensive disease. The mortality rate due to hypertensive disease, heart disease, and cerebrovascular disease increased compared with that in the previous year; among these conditions, ischemic heart disease, including AMI, resulted in a higher mortality rate in males than in females. In a previous study, female AMI patients had a higher mortality rate than males possibly because females were older than males at the time of disease onset [19]. The incidence rates of heart disease, DM, and hypertension in females was also high [20]. Similarly, in the present study, females with and without DM were older than males, and the prevalence rate of underlying diseases was higher in females than in males. Regarding long-term prognosis, females demonstrated a significantly higher mortality rate and incidence of MACE than males.
A European study analyzed the long-term prognosis of patients with AMI and found that the mortality rate was not significantly different between males and females in the age-adjusted analysis [21]. In another study in Europe, no difference was found in the short and long-term mortality rates between male and female AMI patients in PSM analysis [22].
According to the Korean AMI data, females had a significantly higher mortality rate and incidence of MACE than males because female patients tended to be older at the time of disease and have more underlying diseases than male patients [23].
A German study compared the long-term mortality in male and female MI patients with and without DM. In that study, the mortality rate in male and female patients without DM were comparable, but female patients with DM had a significantly higher mortality rate than male patients with DM [24]. In contrast, a study in Finland conducted an age-adjusted analysis of the prevalence of AMI in patients with and without DM and found that males had a significantly higher AMI rate than females [25].
In a European study, the incidence of coronary artery disease was comparable between male and female diabetic patients. However, the incidence of obstructive coronary artery disease was higher in non-diabetic males than in non-diabetic females [26]. Obstructive coronary artery disease has a higher mortality rate than non-obstructive and normal coronary arteries [27]. The results regarding the differences in clinical outcomes between males and females may be related to the intrinsic differences in biology, pathophysiology, and psychosocial factors according to sex [28].
The level of troponin I measured at hospitalization was significantly higher in males than in females in both the diabetic and non-diabetic groups. Troponin I is a myocardium-specific enzyme related to multi-vessel diseases and complex lesions found through coronary angiography [29]. Males with and without DM had significantly more culprit lesions in the left main coronary artery than females; culprit lesions in the left main coronary artery were associated with a high mortality rate in a previous study [30]. In addition, on coronary angiography, type C lesions were significantly more common in non-diabetic males than in non-diabetic females.
For both sexes, factors affecting mortality in the diabetic and non-diabetic groups were old age, heart failure, renal dysfunction, anemia and no PCI. The author also confirmed that the average creatinine level measured at hospitalization was significantly higher in males than in females. Previous studies have also reported that mortality is significantly higher for both cardiac and non-cardiac deaths if the creatinine level is higher than 1.2 mg/dL [31]. In addition, non-diabetic males showed a lower average LVEF than non-diabetic females. In the United States Framingham Heart Study comparing the long-term mortality rates in males and females with heart failure, males had higher mortality rates than females in the age-adjusted and unadjusted analysis [32]. In addition, old age was found to be the independent predictor of mortality, while a preceding study found that old age was a major predictor of mortality in patients with AMI [33]. In particular, the mortality rate in patients with AMI aged ≥ 75 years was found to be higher in males than in females [34].
The present study prospectively enrolled patients with AMI, and some limitations should be considered when interpreting its results. First, since the fasting blood glucose level and HbA1c level were not measured in all patients, patients who were not diagnosed with DM may have been excluded from the diabetic group. Second, it is essential to check whether patients diagnosed with DM after discharge are adhering to the DM treatment regimen.
In conclusion, there was no significant difference in the prognosis of patients with AMI accompanied by DM in terms of sex. However, non-diabetic male AMI patients showed higher mortality and MACE than non-diabetic females AMI patients did.
KEY MESSAGE
Female acute myocardial infarction (AMI) patients with and without diabetes had a higher mortality than male AMI patients with and without diabetes.
After propensity score matching, there was no significant difference in the prognosis of male and female diabetic patients. Mortality and major adverse cardiac events were higher in non-diabetic males than in non-diabetic females.
Old age, renal dysfunction, heart failure, and anemia affected the mortality of the diabetic and non-diabetic groups in both sexes.
Notes
Conflict of interest
No potential conflict of interest relevant to this article was reported.
Acknowledgements
This research was supported by a fund (2013-E63005-02) by Research of Korea Centers for Disease Control and Prevention.