INTRODUCTION
Patients with chronic kidney disease (CKD) associated with cardiovascular disease (CVD) have a higher risk of death than the general population [
1]. Heart failure (HF) associated with CKD increases the risk of death, and these patients have a poor prognosis [
1,
2]. Therefore, in patients with CKD, HF needs to be diagnosed and treated early [
3,
4]. In general, the level of B-type natriuretic peptide (BNP), which reflects an increase in the volume of the left ventricle, is elevated in patients with CKD or end-stage renal disease (ESRD), often in the presence of normal cardiac function [
1]. This means that BNP cannot be used as an accurate marker for the diagnosis of HF in patients in whom the left ventricular (LV) ejection fraction (EF) is preserved. Presently, the ratio of early diastolic mitral inflow velocity to early diastolic mitral annulus velocity (E/e' ratio) is used for the evaluation of LV filling pressure, and it has been used as a marker to diagnose diastolic HF [
5,
6]. In hypertensive patients with elevated E/e' ratio the annual mortality rate is 10% and the ratio is considered to be a prognostic factor for the development of CVD [
3]. However, with respect to the different degrees of CKD associated with HF, studies on the usefulness of the tissue Doppler E/e' ratio as a predictive factor for the development of CVD and mortality have not been conducted. In the present study, we investigated whether the E/e' ratio, which is a marker for the diagnosis of diastolic HF in CKD patients, could predict the incidence of CVD and mortality.
DISCUSSION
CVDs are major causes of death in CKD and ESRD patients [
1]. Among the CVDs, HF increases mortality associated with the cardiovascular system in patients with CKD and ESRD, which means that the prognosis of patients with HF is poor [
1,
2].
HF can be subdivided into systolic HF and diastolic HF. Diastolic HF is defined as cases satisfying more than three of the nine clinical conditions used in the PEP-CHF trial [
7]. The objective test standard was defined as cases that showed two of the following findings in echocardiography: EF > 50%, dysfunction of the left ventricle during the diastolic phase (i.e., enlargement of the left ventricle), abnormal Doppler results for the LV inflow; and E/e' ratio > 10 [
7].
Although the prognosis for diastolic HF is better than for systolic HF, the annual mortality rate is approximately 10%. In addition, this rate is on the increase as the incidences of diabetes and hypertension increase [
3]. Patients with diastolic HF are mostly elderly (age range, 74 to 76 years), and females make up of the majority (62% to 66%) of these cases. Diastolic HF frequently develops in association with several other diseases, such as hypertension (55% to 77%), coronary artery disease (36% to 53%), atrial fibrillation (32% to 41%), diabetes (32% to 45%), CKD (23% to 26%), cerebrovascular diseases (15%), obesity, and anemia [
3]. Diseases associated with diastolic HF are risk factors for CKD and, thus, in patients with CKD, similarly, the incidences of diastolic HF and CVD are increased [
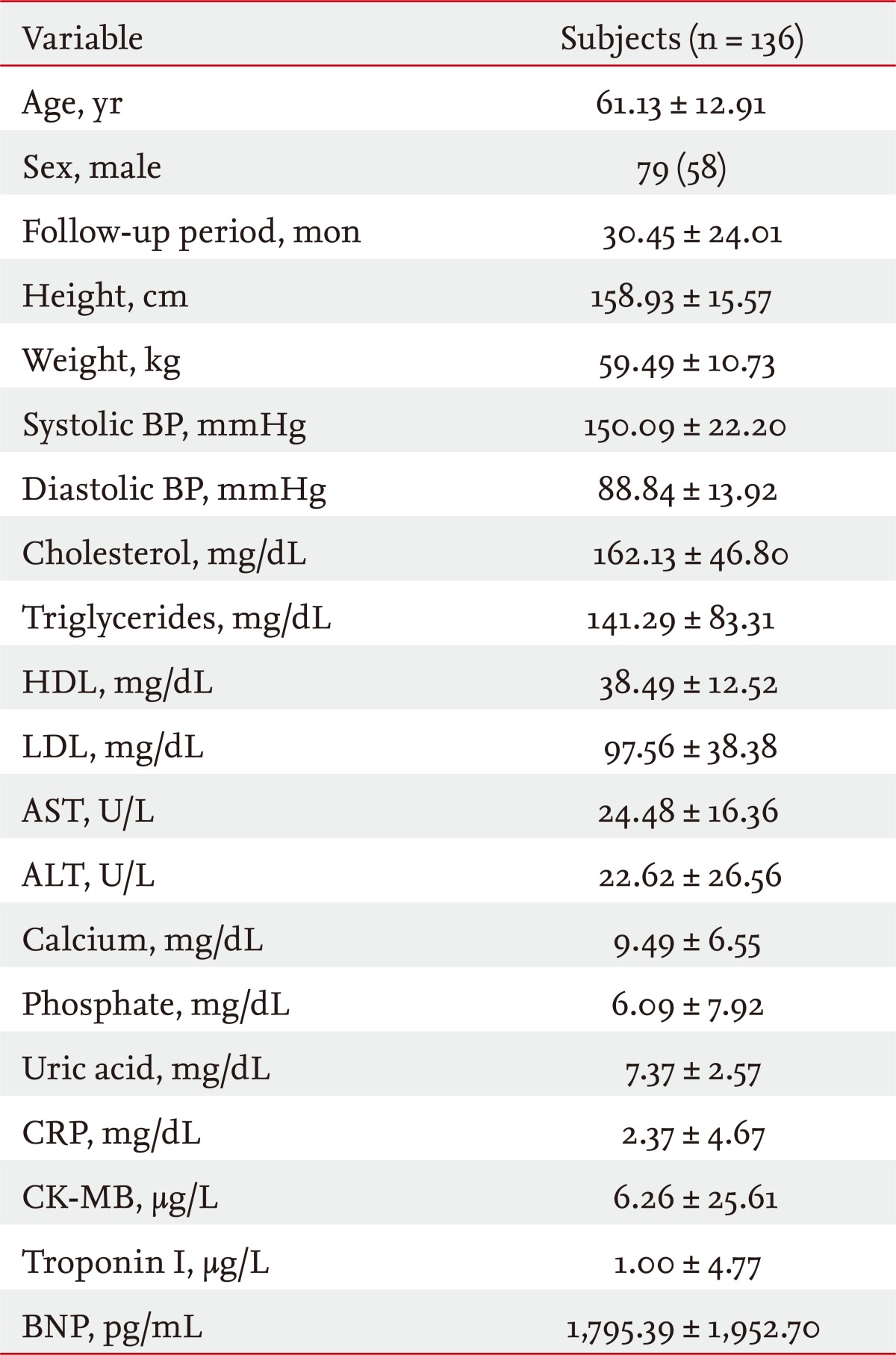
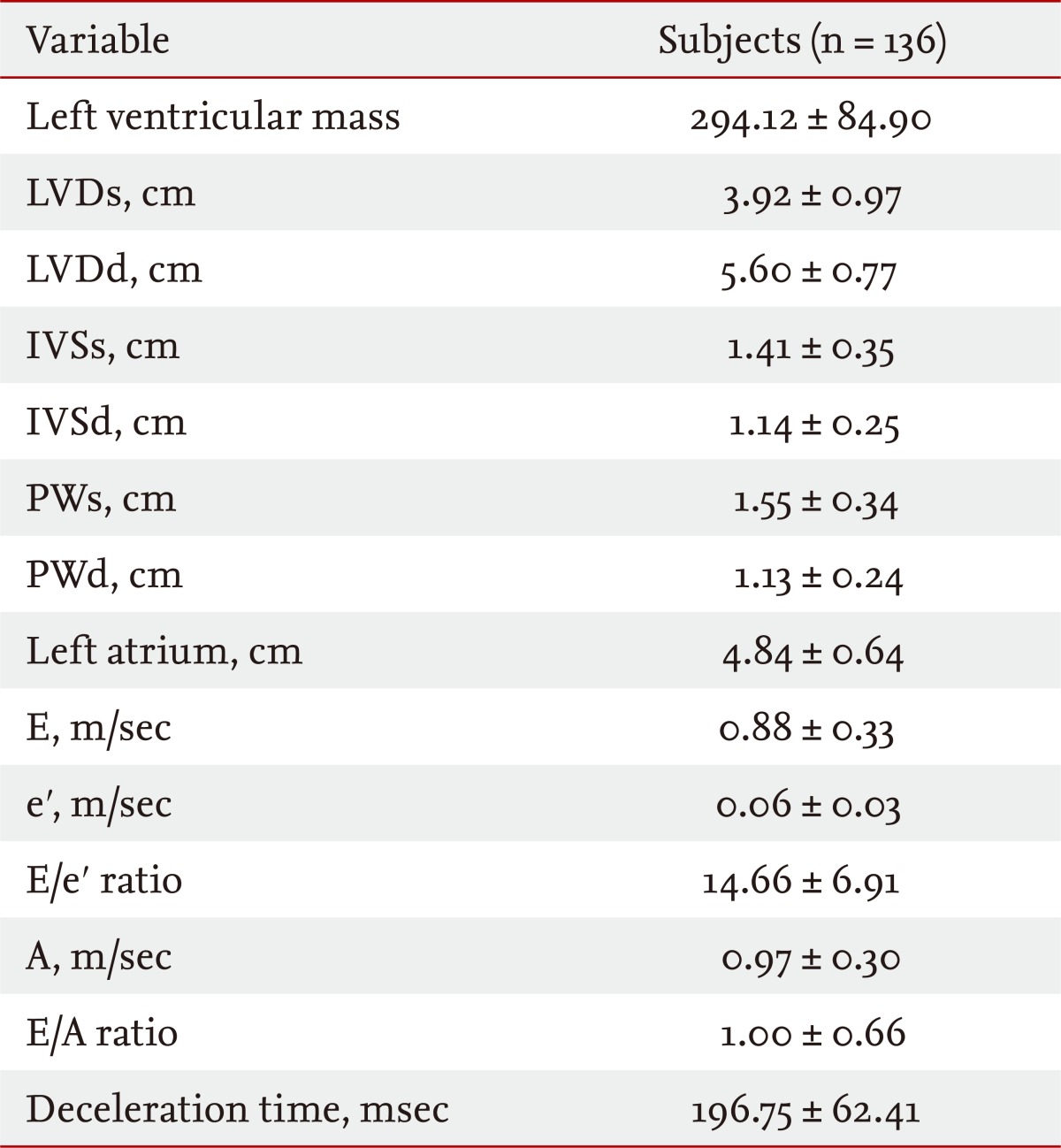
5]. In the present study of 186 patients with CKD who visited our hospital complaining of dyspnea, systolic HF was discovered in 50 patients (36.7%) and diastolic HF was diagnosed in 136 patients (73.1%). Among these, 83 (44.6%) patients had diastolic HF only, and it was found that diastolic HF strongly influenced the etiology of dyspnea.
As reported previously, BNP is a protein that is secreted from heart muscles during hemodynamic overload and, as it has been reported to reflect LV end-diastolic wall stress [
8], it is a widely used marker for the evaluation of diastolic HF and assessment of prognosis. Nonetheless, in patients with CKD with deteriorated kidney function and in patients with ESRD, the levels of BNP are basically increased, which limits its usefulness [
8]. In particular, for patients in whom EF is preserved (in other words, those with diastolic HF) it should be diagnosed carefully. For a more accurate evaluation of heart function, pulmonary capillary wedge pressure (PCWP) was used to evaluate the LV filling pressure. As this involves an invasive procedure, its use is limited. It has been reported that in echocardiography, the E/e' ratio derived from tissue Doppler images correlates significantly with the PCWP measured by invasive methods [
8]. As a result, the E/e' ratio has been used widely to evaluate diastolic HF in patients with HF.
Diastolic HF is diagnosed on the bases of clinical symptoms and echocardiographic assessments of the retained systolic function of the left ventricle and the state of deterioration of diastolic function [
3]. The E/e' ratio is an index that can be used to evaluate the LV filling pressure. It is applied to diagnose diastolic HF [
2,
4,
6]. The E/e' ratio is an index that reflects accurately the LV filling pressure [
6], and it is a predictive factor for the development of CVDs in patients with hypertension [
3,
6]. In patients with myocardial infarction, the E/e' ratio is considered to be a strong predictive factor for survival [
4]. HF is seen in more than 50% of patients with renal failure [
9]. Thus, for patients with CKD and ESRD, it is more important to diagnose HF early and to initiate its treatment [
9].
The E value reflects the status of the mitral valve, as determined by the LV relaxation and the left arterial pressure [
8-
10], and the state of the relaxation of the myocardium can be evaluated by assessing the value of e'. If relaxation of the myocardium is abnormal, not only the magnitude of e' is decreased but also the time of opening of the mitral valve is delayed [
8-
10]. An E/e' ratio < 8 is considered to be normal, and a ratio > 15 is considered to reflect an increase in the LV filling pressure [
11-
13]. In patients with normal EF, tissue Doppler echocardiography has been used to evaluate LV filling pressure and LV stiffness [
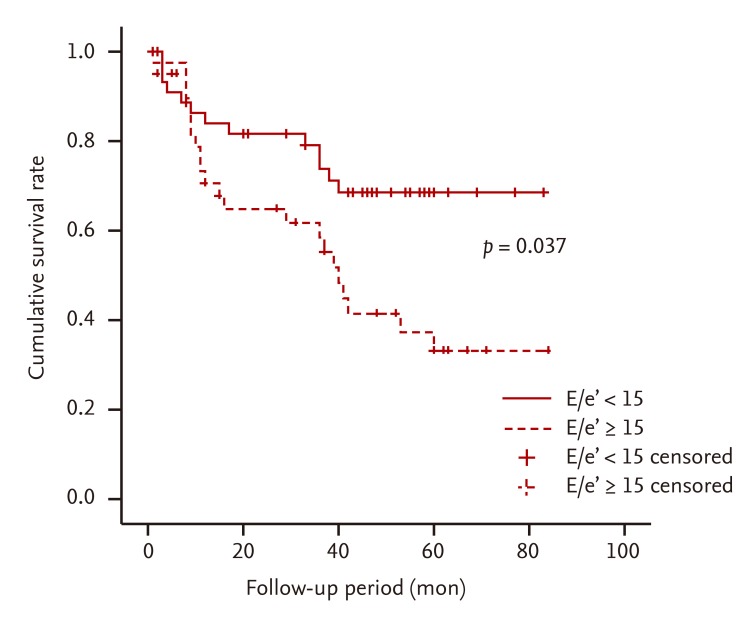
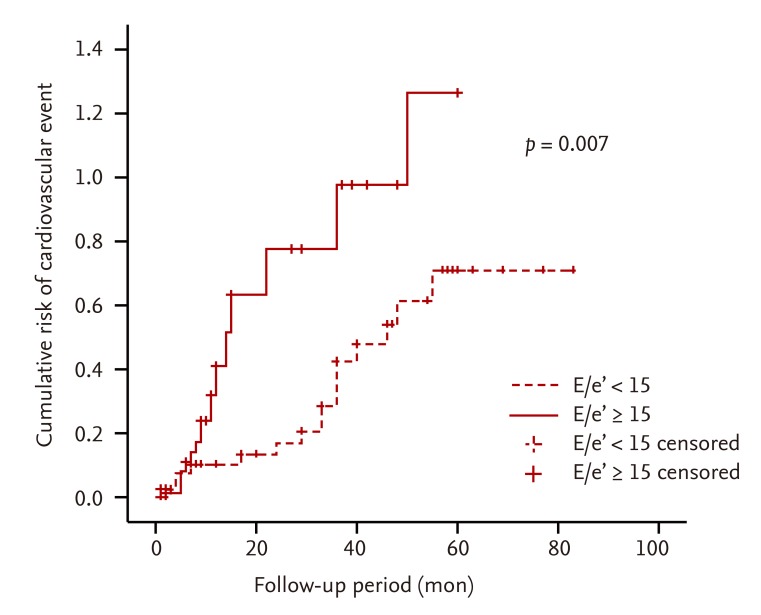
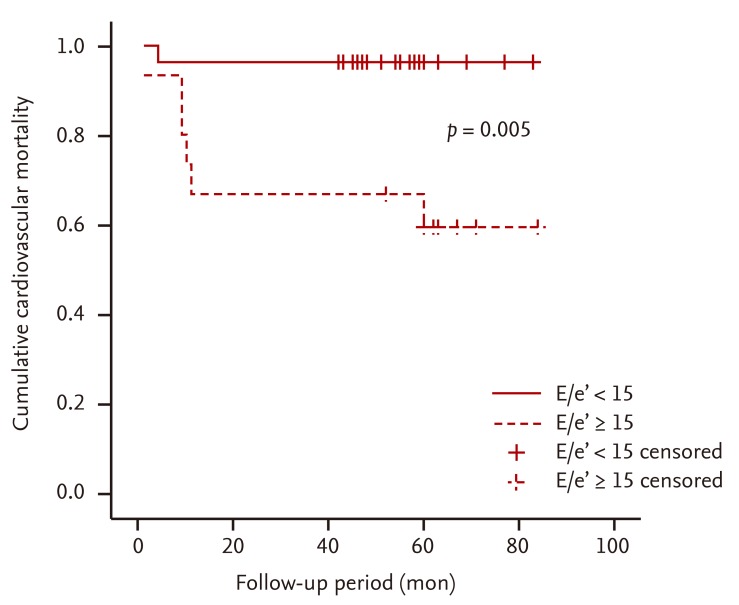
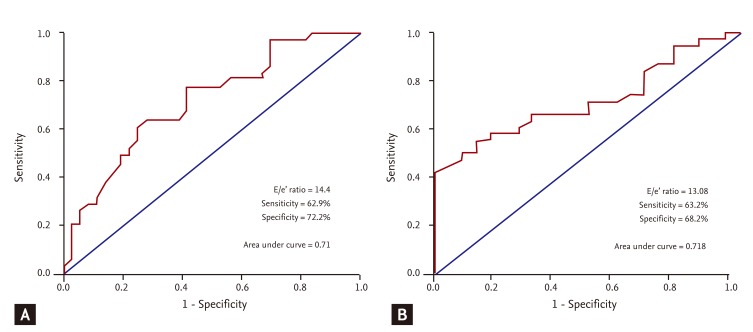
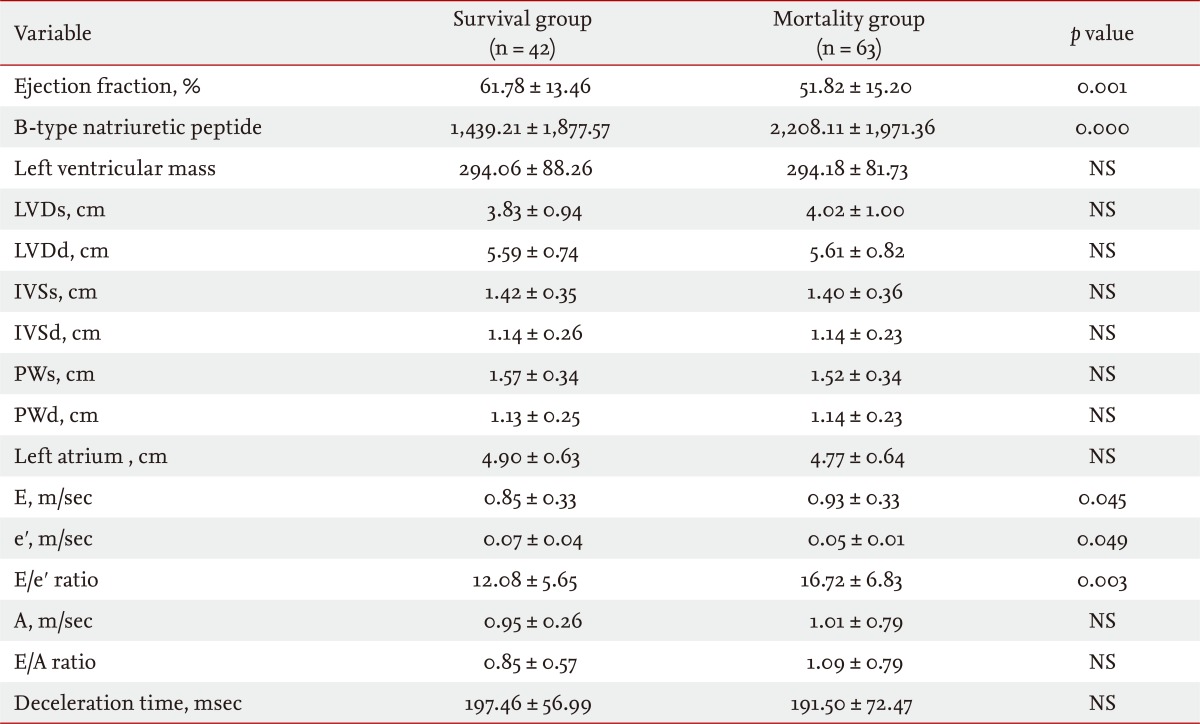
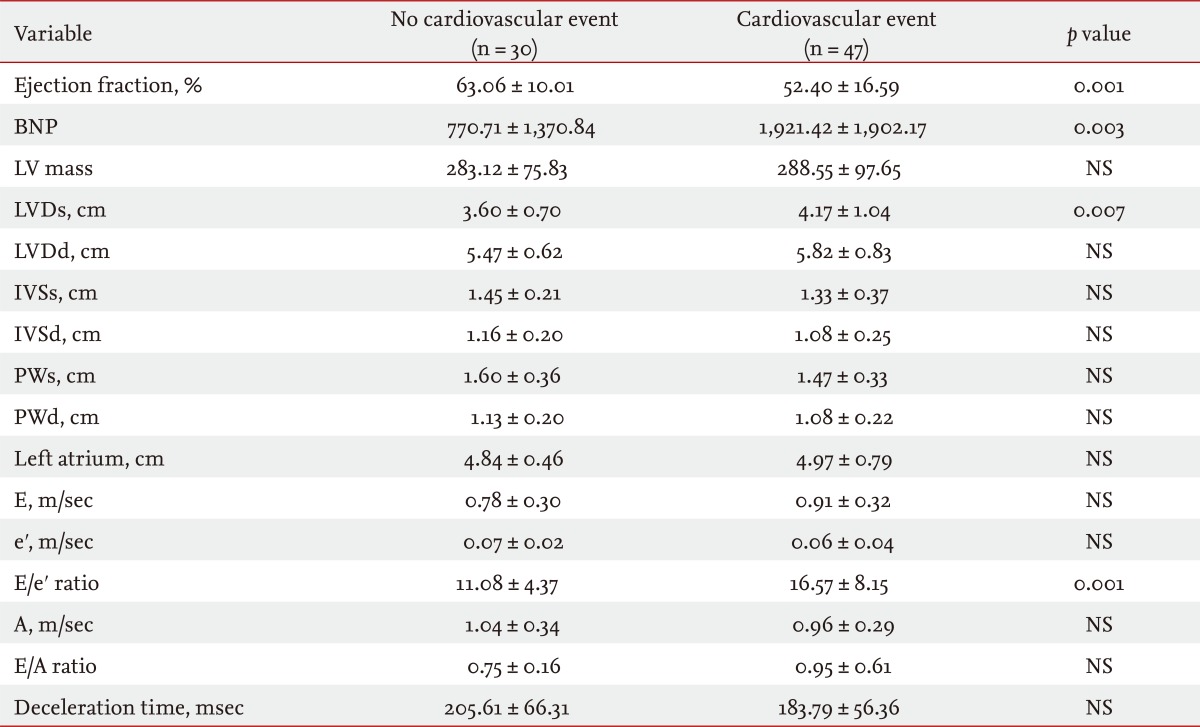
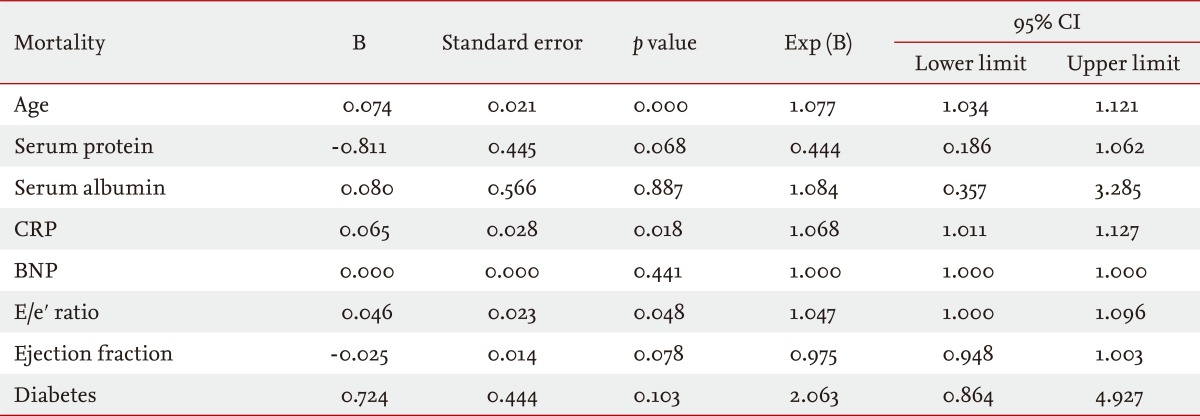
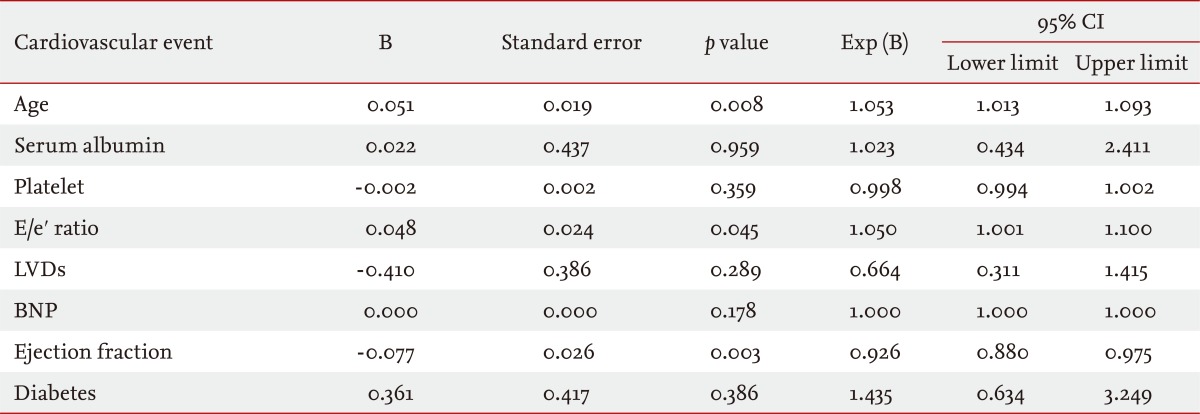
11]. The results of the present study show that, in patients with an E/e' ratio > 15, the incidences of mortality and CVD are statistically significant, whereas the LV EF, GFR, and BNP are not significant. Therefore, in CKD patients, an increase in the E/e' ratio may increase mortality, as well as the development of CVD without any association with factors that increase systolic HF and BNP (
Figs. 2 and
3). In addition, in patients with CKD associated with diastolic HF, age, CRP, and the E/e' ratio were found to be factors that predict mortality. Age, EF, and the E/e' ratio were found to be factors that predict the incidence of CVD. In particular, the E/e' ratio was found to be predictive of both mortality and the incidence of CVD (
Tables 5 and
6).
In patients with CKD, hypertension frequently induces diastolic failure and induces ventricular hypertrophy, myocardial dysfunction, fibrosis due to the deposition of collagen in connective tissues, and myocardial ischemia [
14]. CKD is associated with hypertension in many cases due to several factors and, regardless of the stage of CKD, deterioration of diastolic function may be an associated phenomenon. Therefore, regardless of the level of deterioration of renal function, screening by echocardiography is required. Considering that the E/e' ratio and the level of renal failure were not correlated in a statistically significant manner, echocardiography should be performed for patients with CKD, and the association with diastolic failure should be assessed. For patients with major risk factors for the induction of CKD, such as diabetes and hypertension, evaluation of the E/e' ratio by echocardiography is crucial [
15,
16]. In patients with CKD, for the diagnosis of asymptomatic diastolic failure, an E/e' ratio > 11 (assessed by tissue Doppler echocardiography) is considered to correspond to PCWP > 15 mmHg [
8,
12,
13]. Application of the E/e' ratio would facilitate the early diagnosis of these patients, as well as the early diagnosis of diastolic HF and early initiation of treatment, and would ameliorate the deterioration of renal failure and the deterioration of HF caused by cardio-renal syndrome [
17-
19]. In the present study, E/e' ratios of 14.40 and 13.08 in the ROC curve were predictive of mortality (62.9% sensitivity, 72.3% specificity) and the incidence of CVD (63% sensitivity, 68.2% specificity). In patients with CKD or ESRD, it may be useful to apply lower E/e' ratios than the currently used value of 15 (
Fig. 5).
In conclusion, diastolic HF is an important factor that increases mortality related to the cardiovascular system in patients with CKD whose extent of kidney function deterioration differs [
20]. As a non-invasive method to allow early assessment, the E/e' ratio could be applied usefully. For the diagnosis of HF in patients with CKD and the evaluation of responses to treatments, further studies using more accurate, non-invasive, simple, and highly reproducible measurement methods are required.





 PDF Links
PDF Links PubReader
PubReader ePub Link
ePub Link Full text via DOI
Full text via DOI Download Citation
Download Citation Print
Print



