Musculoskeletal complications in patients with diabetes mellitus
Article information
Abstract
Musculoskeletal conditions are common in patients with diabetes. Several musculoskeletal disorders are viewed as chronic complications of diabetes because epidemiological studies have revealed high correlations between such complications and diabetes, but the pathophysiological links with diabetes remains unclear. Genetic predispositions, shared risk factors, microvascular impairments, progressive accumulation of advanced glycation end-products, and diabetic neuropathy may underlie the development of musculoskeletal disorders. Musculoskeletal complications of diabetics have received less attention than life-threatening microvascular or macrovascular complications. Here, we review several diabetic musculoskeletal complications with a focus on the clinical importance of early recognition and management, which would improve quality of life and physical function.
INTRODUCTION
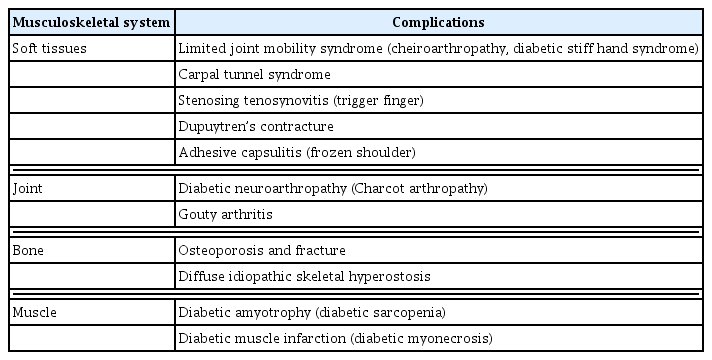
Diabetes mellitus is a chronic disease that imposes enormous socioeconomic burdens attributable to complications of various bodily systems. Diabetes affected 463 million people (9.3% of all people) in 2019 and will affect 700 million (10.9%) by 2045 [1]. In 2018, the prevalence of diabetes among Korean adults aged 30 years and older was 13.8% [2] and the 2019 healthcare costs were about 18 billion dollars [3]. The life expectancy of diabetics is increasing due to the development of novel antidiabetic drugs and medical techniques. This means that the burden of diseases reflecting the chronic complications of diabetes will also increase [4]. Macrovascular and microvascular complications directly threaten survival. Early recognition, prevention, and treatment of such complications have been prioritized. Epidemiologically, musculoskeletal disorders (MSDs) are recognized chronic complications [5] but have received less attention than the life-threatening vascular complications. Painful MSDs significantly compromise quality of life (QoL). However, such conditions are very treatable; early diagnosis and treatment of MSDs improve QoL [6]. Here, we review the relevant MSDs (Table 1).
FIBROPROLIFERATIVE COMPLICATIONS OF SOFT TISSUES
Possible pathophysiological mechanism and clinical considerations
It remains unclear why diabetes is associated with pathophysiological fibroproliferative complications in soft tissues. Many studies have found that elevated levels of advanced glycation end-products (AGEs) are associated with the microvascular complications of diabetes [7,8]. Abnormal AGE accumulation may trigger fibroproliferative complications [9]; proteins such as collagen that exhibit low biological turnover rates may be particularly susceptible to glycation [10]. Boivin et al. [11] showed histologically that the maximal tendon load, tensile stress, stiffness, and elasticity were low in an animal model of diabetes. Reddy et al. [12,13] reported that in rabbit tendons AGE cross-linking reduces sensitivity to collagenase and remodeling capacity, and increases stiffness. An inflammatory response can also trigger fibroproliferative complications in diabetics. Chondrocytes and tendon cell membranes host a specific AGE receptor [14]. Franke et al. [15] found that AGEs enhance transcription of the nuclear factor kappa-light-chain enhancer of activated B cells (NF-κB) and upregulate the production of pro-inflammatory mediators including tumor necrosis factor-α (TNF-α) and interleukin-6 (IL-6). The levels of cytokines and vascular endothelial growth factors increase in the rotator cuffs of diabetics [16]. Increased levels of reactive oxygen species in hyperglycemic environments trigger inflammatory cascades and induce cell damage caused by various cytokines and growth factors [17].
It is clear that fibroproliferative and microvascular complications are linked; the latter should be examined if the former are present [18,19]. As is true of other diabetic complications, strict glycemic control may prevent the onset of such complications and/or delay progression but not completely reverse them [20]. No treatment that reverses pathological disease progression is yet available. Initial conservative treatments seek to control pain and limitations of motion. Surgery is possible if a response is lacking, and when an irreversible deformity develops.
Limited joint mobility syndrome (cheiroarthropathy; “diabetic stiff hand syndrome”)
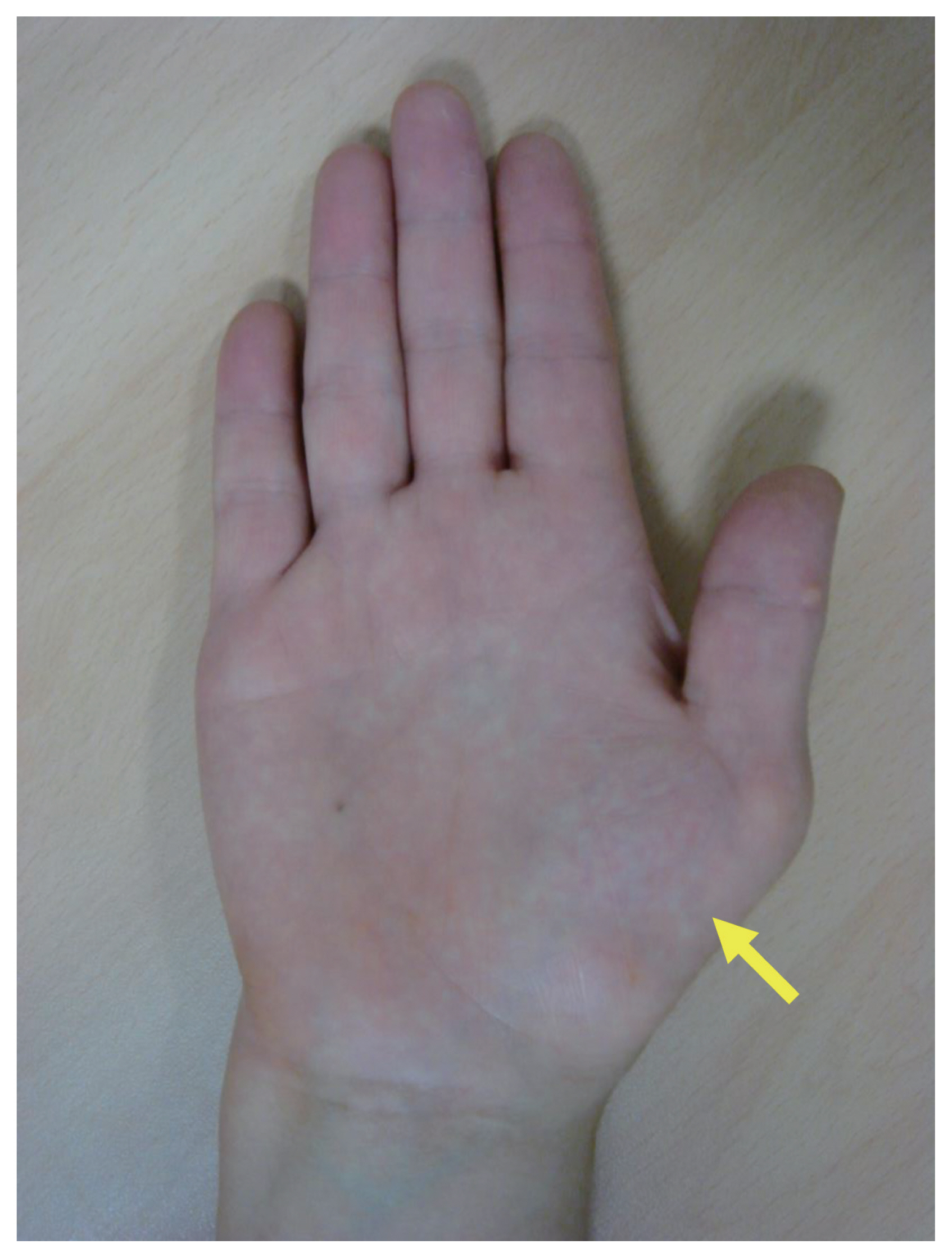
Limited joint mobility syndrome (LJMS) is characterized by limited motion of the small hand and finger joints [21]. Stiff hands in patients with longstanding diabetes were first described by Lundbaek in 1957 [22]. The prevalence of LJMS is 8% to 58% in patients with type 1 diabetes mellitus (T1DM) and 25% to 76% in those with type 2 diabetes mellitus (T2DM); the rate in general populations is 1% to 20% [23]. The symptoms include painless stiffness, fixed flexion contracture, impaired fine movement, and decreased grip strength (both hands and fingers) [24]. The skin of the dorsum of the hand may become thick and waxy prior to motion limitation [25]. Helpful clinical features include the “prayer sign” and the “tabletop sign.” The prayer sign is present when the entire surface of the hand cannot be appressed when the palm and fingers contact the wrist during dorsiflexion (Fig. 1A). The tabletop sign is positive if the palmar surface does not fully touch the table, rather falling away when the palm contacts the tabletop at a right angle (Fig. 1B) [26]. Diseases such as osteoarthritis, rheumatoid arthritis, scleroderma, and systemic lupus erythematosus must be excluded [25]. LJMS can also develop in joints other than the fingers. For example, LJMS in the small joints of the foot may increase the risk for falls or diabetic foot ulcers [27,28]. Daily stretching exercises may help slow the progression of joint stiffness, and analgesics or corticosteroid injections may relieve pain or joint contracture [29,30]. Surgery may be necessary if such contracture or a deformity is severe [30].

Clinical signs of limited joint mobility syndrome. The “prayer sign” (A) and the “tabletop sign” (B) in a middle-aged woman with long-term type 2 diabetes. The prayer sign reflects an inability to appress the flattened palms (as when praying). The tabletop sign reflects an inability to place the complete palm on the surface of a table with the wrist at a right angle.
Carpal tunnel syndrome
Carpal tunnel syndrome (CTS) is the most common entrapment neuropathy caused by compression of the median nerve within the osteofibrous canal (the carpal tunnel) [31]. Diabetes is a major risk factor for CTS; the prevalence is much higher (14% to 30%) in diabetics than general populations (3.8%) [32,33]. A meta-analysis of 18 studies involving > 37 million individuals found that the pooled odds ratio (OR) for diabetic patients was 1.69 (95% confidence interval [CI], 1.45 to 1.96) [34]. In a recent cohort study using a National Diabetes Register containing data on approximately 1.1 million residents of Sweden, the prevalence ratios of CTS among patients with T1DM and T2DM compared to those without diabetes were 3.7–4.5 and 2.0–2.5, respectively [35]. Nerve compression triggers typical paresthesia of the thumb, index finger, middle finger, and the radial side of the ring finger, causing thenar muscle weakness and atrophy of the affected finger in severe cases (Fig. 2) [36]. Physical examinations that identify paresthesia in the median nerve include tapping on the median nerve of the wrist (the Tinel test), full palmar flexion of the wrist for more than 1 minute (the Phalen test), and raising the hand over the head for more than 1 minute (the hand elevation test). The symptoms may improve when the wrist is shaken or flicked (the flick sign). If CTS is clinically suspected, the condition can be confirmed electrophysiologically; the focal nerve conduction velocity is decreased at the entrapment site [36]. Recently, high-resolution ultrasound has been used to verify compression and morphological change in the median nerve [36]. Corticosteroid injections help relieve CTS symptoms [37]. Surgical decompression is the treatment of choice for patients evidencing severe nerve damage in nerve conduction studies if the etiology is not reversible [38]. Diabetic patients are 4- to 14-fold more likely to require surgery than general populations [39].
Stenosing tenosynovitis (trigger finger)
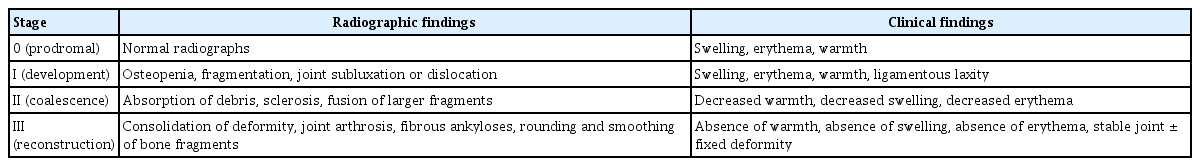
Stenosing tenosynovitis (commonly termed trigger finger) is caused by inflammation attributable to repeated friction between the flexor tendon and the sheaths that form the tunnel affording mechanical stability to that tendon [40]. Inflammation causes the tendon and sheaths to swell and form nodules. The flexor tendon becomes trapped in the tunnel, and the finger joint is then locked in flexion (Fig. 3A) [41]. The prevalence in diabetic patients is 5% to 20%, much higher than the 1% to 2% in general populations [42]. Unlike in such populations, trigger finger in diabetics is more common in women and is characterized by bilateral and multiple finger involvement [43]. Extensor stretching exercises can help prevent recurrence [44]. Immobilization is preferred in the acute phase, and local corticosteroid injections can be considered in severe cases [45]. If conservative treatments fail, open surgery releases the A1 pulley [45].
Flexion contractures in patients with stenosing tenosynovitis (trigger finger) (A) and Dupuytren’s contracture (B). Yellow arrows indicate fingers locked in the flexed position in patients with severe stenosing tenosynovitis (trigger finger) (A) and Dupuytren’s contracture (B); it was impossible to straighten the fingers. The white arrow in (B) indicates thickened finger tissue.
Dupuytren’s contracture
Dupuytren’s contracture (DC) is a progressive condition; nodules or contractures form in the palmar fascia, caused by fibrosis. The incidence of DC in diabetic patients is about 16% to 42% [46] and is related to the duration of diabetes, old age, the male sex, smoking, and alcohol consumption [47]. Initially, nodules develop near the metacarpophalangeal joint on the palmar side, creating a fibrous band with the finger, resulting in flexion contracture and limited movement (Fig. 3B) [48]. DC principally affects the fourth and fifth fingers (unlike trigger finger, which affects primarily the thumb and the index and middle fingers) [48]. Local corticosteroid injections may be considered if tenderness is evident or the nodule grows [46]. Intralesional, clostridial collagenase injections relieve the contractures and improve joint movement [49]. Surgery may be considered if joint movement is impaired by progressive flexion contracture [46]. Recurrence after surgery is more frequent in diabetic patients [50].
Adhesive capsulitis (frozen shoulder)
Adhesive capsulitis (AC), also termed “frozen shoulder” (by the American Academy of Orthopedic Surgeons), is “a condition of varying severity characterized by the gradual development of global limitation of active and passive shoulder motion where radiographic findings other than osteopenia are absent” [51]. AC is triggered by inflammation that in turn causes fibrosis of the glenohumeral joint capsule and adhesion of surrounding structures [52]. Diabetes is a significant risk factor for AC; the prevalence in diabetics is 19% to 29%, much higher than the approximately 5% in general populations [53,54]. Old age, long diabetes duration, and poor glycemic control increase its prevalence, and the prognosis is poorer in diabetics than general populations [53,55]. It is accompanied by progressive stiffness and significant restriction of the range of motion [56]. Pain or a limited range of motion develop during sudden movements such as shoulder external rotation or abduction [57]. Diagnosis is based primarily on clinical symptoms and physical examination. As the incidence of rotator cuff tendinopathy is also approximately 1.5-fold higher in diabetics than general populations, this condition should be considered during differential diagnosis of AC [58,59]. Non-contrast, shoulder magnetic resonance imaging (MRI) aids the differential diagnosis [60]. Most cases of AC resolve over time; physiotherapy and oral analgesics may accelerate symptom relief [61]. Local corticosteroid injections and hydrodilatation are useful adjunctive treatments [61,62]. Surgery may be required if conservative treatments elicit no response [61]. Diabetics evidence more severe symptoms than general populations and require early and frequent intensive management [57].
JOINT COMPLICATIONS
Diabetic neuroarthropathy (Charcot arthropathy)
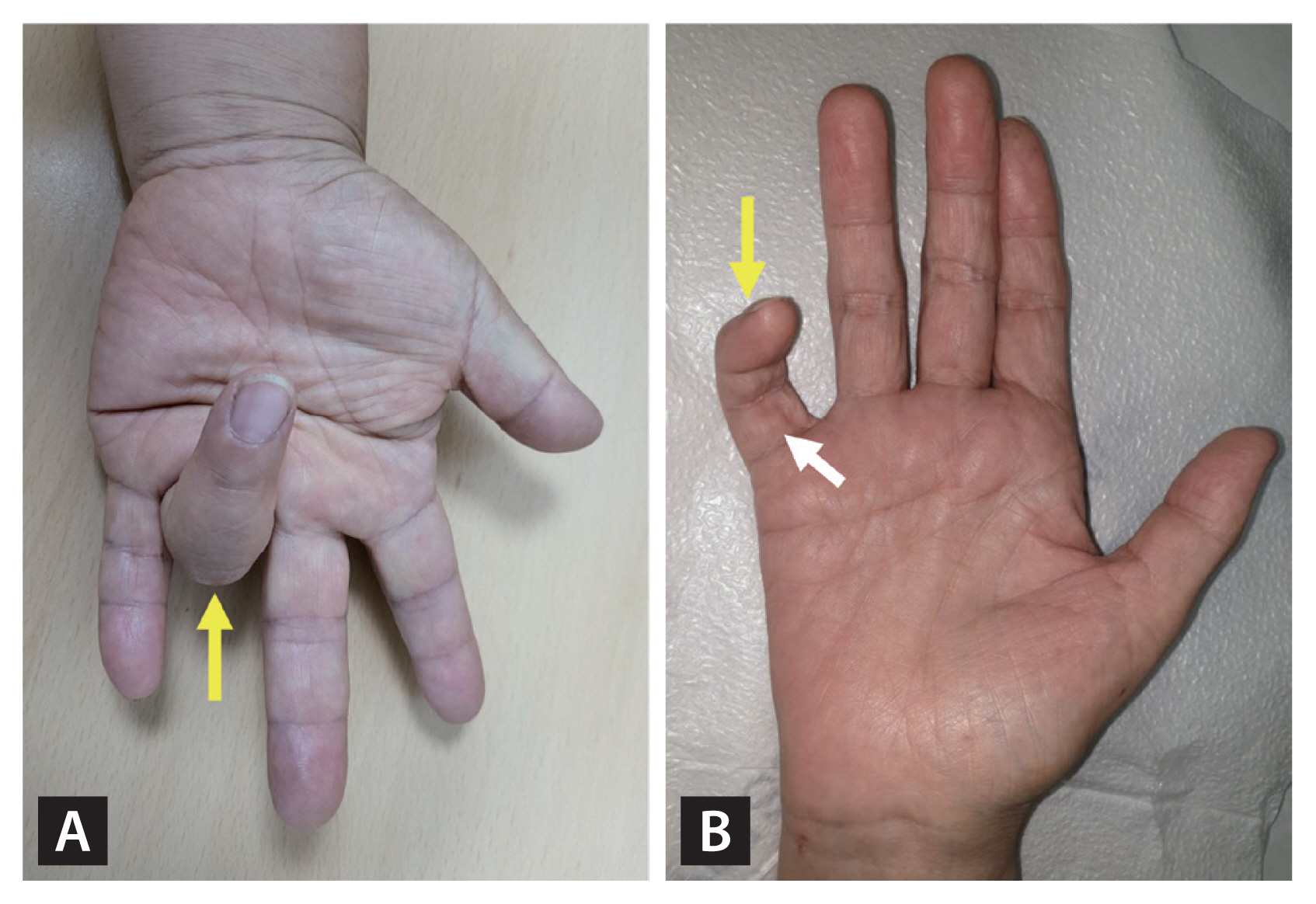
Neuropathic arthropathy, also termed Charcot arthropathy, is a progressive and destructive disease of the joints and adjacent bony structures caused by loss of sensation [63]. Charcot described the prototype of the disorder in the context of the tabes dorsalis [64]. Similar changes occur in patients with diabetic neuropathy, which is then termed diabetic neuroarthropathy (DN). Peripheral or autonomic neuropathies (microvascular complications of diabetes) can trigger mechanical or vascular joint changes; bone metabolic abnormalities seem to be associated with DN development [65]. The prevalence of DN is 0.1% to 7.5% in diabetic patients but 29% to 35% in those with diabetic peripheral neuropathy [66]. DN principally affects the foot and ankle joints; the symptoms include painless joint swelling, warmth when touched, instability, and deformity (Fig. 4) [65]. The physician should suspect DN when unilateral warmth, swelling, and erythema develop in a patient with diabetes of long duration and diabetic neuropathy. Infections (cellulitis, septic arthritis, or osteomyelitis), gout, osteoarthritis, and rheumatoid arthritis should be excluded [67]. Structural changes in the feet change weight-bearing and then trigger local trauma such as diabetic foot ulcers. The DN staging system of the modified Eichenholtz classification aids management (Table 2) [68]. Plain radiography may reveal the typical (stage-specific) findings of DN and MRI assists the differential diagnosis. In the acute phase, the most critical intervention is avoidance of foot weight-bearing by applying a cast or the use of crutches or a wheelchair [69]. Prevention of diabetic foot ulcers and infections is essential in patients exhibiting chronic and severe joint damage [69]. Surgical treatment may be considered if plantar stability cannot be maintained using special footwear or an orthosis to counter the foot deformity. However, surgery is best avoided [70].

Foot deformities in a patient with diabetic neuroarthropathy (Charcot arthropathy). Patients with diabetic neuropathy may exhibit various foot deformities depending on the locations of the microfractures. As shown in this photograph, the toes may be curved to the medial side (yellow arrow) or be clawlike (white arrows).
Gouty arthritis
Gout is an inflammatory form of arthritis in which monosodium urate crystals are deposited in the joints because of hyperuricemia [71]. Gout and diabetes interact in that each condition increases the incidence of the other, reflecting the correlation between hyperuricemia and insulin-resistance [72]. Although gout is a well-known major risk factor for diabetes [65], whether diabetes increases the risk for gout remains controversial. In a large, 3-year, community-based observational study, gout developed in 16.0% of patients with T2DM and 14.2% of those with prediabetes; the figures were significantly higher than the 2.7% of the general population [73]. In another prospective observational study, the relative risk for gout development in diabetics was as low as 0.77 (95% CI, 0.60 to 0.97) [74]. It may be that diabetes does not directly increase the risk for gout. Rather, the two conditions co-occur because they share risk factors or clinical features related to metabolic syndrome [75]. Gout exhibits two phases: recurrent acute inflammatory arthritis (Fig. 5) and chronic tophaceous gout [71]. During acute episodes, nonsteroidal anti-inflammatory drugs (NSAIDs), corticosteroids, or colchicine are used to reduce acute inflammation. Patients evidencing recurrent acute attacks, gouty tophi, urinary stones, and radiologically confirmed damage are prescribed long-term urate-reducing agents such as probenecid, allopurinol, or febuxostat [76].
SKELETAL COMPLICATIONS
Osteoporosis and fracture
Osteoporosis is a skeletal disorder; bone strength is compromised by a decreased bone mass and microarchitectural damage, increasing the fracture risk [77]. Most epidemiological studies have reported increased risk for fragility fractures in diabetics. Bone mineral density (BMD) decreases in T1DM patients but increases in those with T2DM; however, the fragility fracture risks are enhanced in both T1DM and T2DM patients [78]. The fact that an increased BMD is nonetheless associated with a higher fracture risk in T2DM patients renders risk assessment and fracture prevention challenging. A recent meta-analysis of observational studies found that the relative risk for fracture in young and middle-aged adults with T1DM is 1.88 (95% CI, 1.52 to 2.32) [79] and that in adults with T2DM it is 1.31 (95% CI, 1.17 to 1.46) [80]. In the Women’s Health Initiative Observational Study, patients with T2DM exhibited a higher BMD, but the relative risk for any fracture was 1.20 (95% CI, 1.11 to 1.30) even after controlling for age, weight, fall frequency, tobacco and alcohol use, and exercise [81].
Any effect of glycemic control on the fracture risk remains controversial. Although strict glycemic control did not reduce that risk in the Action to Control Cardiovascular Risk in Diabetes (ACCORD) study [82], a large community-based observational study showed that the fracture risk was 24% to 63% higher in patients with poor glycemic control compared to those with low hemoglobin A1c (HbA1c) levels [83,84]. The duration of diabetes was also a risk factor. The relative risk for hip fracture in patients who were diabetic for more than (vs. less than) 10 years was 1.19 (95% CI, 1.13 to 1.25) [85]. Diabetes-related complications increase the risk for fracture. In a study that used data from a Danish registry, the fracture risk was higher in patients with T2DM accompanied by diabetic retinopathy (OR, 2.08; 95% CI, 1.80 to 2.41), nephropathy (OR, 2.02; 95% CI, 1.65 to 2.47), neuropathy (OR, 1.91; 95% CI, 1.64 to 2.21), or macrovascular complications (OR, 1.92; 95% CI, 1.61 to 2.28), compared to those with no complications (OR, 1.43; 95% CI, 1.35 to 1.50) [86].
The pathophysiology of bone fragility in diabetics is complicated. Most patients with T1DM exhibit complete β-cell failure and low levels of IGF-1 that reduce the peak bone mass when young because osteoblast function is impaired during growth [87]. Pro-inflammatory cytokines, adipokines, glucotoxicity, and AGEs inhibit Wnt signaling. In T2DM patients, skeletal microvascular changes are thought to render osteocyte function and collagen synthesis abnormal, and to decrease bone turnover [88]. Complications such as neuropathy, balance disturbances, sarcopenia, vision impairment, and hypoglycemic events increase the risk for falls and consequent fractures [89].
Of the various glucose-lowering medications, some increase the fracture risk. For example, thiazolidinediones (TZDs) activate peroxisome proliferator-activated receptors and impair osteoblastogenesis, decreasing the BMD and increasing fracture risk. A meta-analysis of 10 randomized controlled trials and two observational studies reported an increased risk for fracture in women treated with TZDs (OR, 2.23; 95% CI, 1.65 to 3.01) [90]. In the Canagliflozin Cardiovascular Assessment Study (CANVAS), of the sodium-glucose cotransporter-2 (SGLT-2) inhibitors, canagliflozin caused hip bone loss and increased the hip fracture risk (hazard ratio [HR], 1.26; 95% CI, 1.04 to 1.52) [91]. Conversely, the incidence of fractures did not increase in the Canagliflozin and Renal Events in Diabetes with Established Nephropathy Clinical Evaluation (CREDENCE) trial (HR, 0.98; 95% CI, 0.70 to 1.37). In other studies, dapagliflozin and empagliflozin did not increase fracture incidence (dapagliflozin [HR, 1.04; 95% CI, 0.91 to 1.18]; empagliflozin: 3.9% and 3.8% in the placebo and empagliflozin groups, respectively) [92,93]. In a recent meta-analysis of 30 randomized controlled trials, the pooled OR of bone fractures was 0.86 (95% CI, 0.70 to 1.06) [94].
There is no specific guideline for osteoporosis management in diabetics. The pharmacological treatments and fall-prevention strategies for diabetics at high risk for fracture are the same as those for osteoporotic patients without diabetes. However, T2DM patients are at increased fracture risk even if the BMD does not decrease. Thus, novel strategies for preventing fragile fractures in patients with T2DM are required; these should differ from those for osteoporosis patients without T2DM but a low BMD. More active fracture risk assessment and earlier medical intervention should be considered in patients with diabetes of long duration or microvascular complications, and those at higher risk for falls because of recurrent hypoglycemia or neurological abnormalities [95].
Diffuse idiopathic skeletal hyperostosis
Diffuse idiopathic skeletal hyperostosis (DISH) is characterized by calcification and ossification of the anterolateral ligaments of the spine [96]. The etiology of DISH remains unknown, but several studies have revealed epidemiological correlations with diabetes. The prevalence of DISH in diabetics is 5% to 50%, higher than in general populations [97]. DISH is most common in the thoracic spine and is diagnosed when calcification of four or more consecutive vertebral ligaments is evident [98]. However, narrowing of the intervertebral space, inflammation of the sacroiliac joint, and signs of degenerative disease or inflammatory spondyloarthropathy must be excluded [99]. Most patients progress slowly and are asymptomatic, but symptoms such as spinal stiffness, lower back pain, limited movement, or compression of surrounding organs may develop [100]. Physiotherapy or NSAIDs may be used to treat pain and stiffness [100]. If there is no response, local corticosteroid injections may help [101]. Surgical treatment may be required if myelopathy, neuropathy, or dysphagia develop because of compression of surrounding organs [101].
MUSCULAR COMPLICATIONS
Diabetic amyotrophy (diabetic sarcopenia)
Sarcopenia is characterized by a progressive deterioration of muscle mass and function with aging. Several medical conditions may accelerate progression, which is closely related to insulin-resistance, impaired fasting glucose levels, and diabetes [102]. The Health, Aging and Body Composition Study showed that deterioration of muscle mass and muscle strength accelerated in elderly diabetics (compared to non-diabetics) exhibiting poor glycemic control (HbA1c > 8%) for at least 6 years [103]. In another study, elderly women with T2DM exhibited about twice as much muscle mass loss than non-diabetic women after 6 years of follow-up [104]. In a study of 414 Koreans more than 65 years old, sarcopenia development was two to four times greater in a T2DM group than a control group [105]. In the Korean Frailty and Aging Cohort Study that enrolled 2,403 elderly women aged 70 to 84 years, those exhibiting insulin-resistance or diabetes (14.7% and 8.5%, respectively) evidenced twice as much sarcopenia than others [106]. Conversely, sarcopenia is a risk factor for diabetes [107]. The U.S. National Health and Nutrition Examination Survey (NHANES) III data revealed that the higher the muscle mass, the lower the extent of insulin-resistance and the lower the risk for diabetes regardless of obesity status [108,109]. The Korea National Health and Nutrition Examination Survey IV (KNHANES IV) found a significant association between insulin-resistance and sarcopenia [110]. Another Korean study on 493 healthy adults (180 men and 313 women) reported that the homeostatic model assessment of insulin-resistance was negatively correlated with muscle mass [111]. The possible pathophysiological mechanisms of sarcopenia in older patients with diabetes include decreased anabolic activity attributable to increased insulin-resistance [112], upregulation of inflammatory cytokines such as TNF-α or IL-6, and/or mitochondrial dysfunction [113].
Diabetic muscle infarction (diabetic myonecrosis)
Diabetic muscle infarction (DMI) is a spontaneous ischemic necrosis of skeletal muscle in the absence of an arterial thromboembolism or an atherosclerotic occlusion of a large artery [114]. It is a rare complication of patients with both longstanding diabetes and multiple microvascular or macrovascular complications [115]. It affects principally the calf and thigh muscles, accompanied by muscle pain and swelling [116]. Nonspecific increases in the levels of muscle enzymes such as creatine kinase, the leukocyte number, the C-reactive protein level, and the erythrocyte sedimentation rate may be noted [116]. When diagnosing DMI, acute arterial occlusion, infection, and a malignant tumor must be excluded. Plain radiography, ultrasound, and MRI may aid diagnosis, but a muscle biopsy may be required [117]. Low-dose aspirin is the preferred antiplatelet treatment (this prevents ischemia progression), but clopidogrel is an alternative; NSAIDs allow of short-term pain relief and other pain relievers can be prescribed if aspirin side effects are of concern [116].
CONCLUSIONS
MSDs in patients with diabetes are more common than in general populations, although the disorders are not confined to diabetics. The disorders significantly impact QoL and the activities of daily living. Early evaluation and management of musculoskeletal problems in diabetics reduce pain, improve QoL, and minimize morbidity and mortality. It is important to consider the clinical characteristics, diagnoses, and treatments of musculoskeletal complications when comprehensively managing diabetes.
Notes
No potential conflict of interest relevant to this article was reported.