 |
 |
|
|
|
Abstract
Background/Aims
Methods
Results
Figure 1
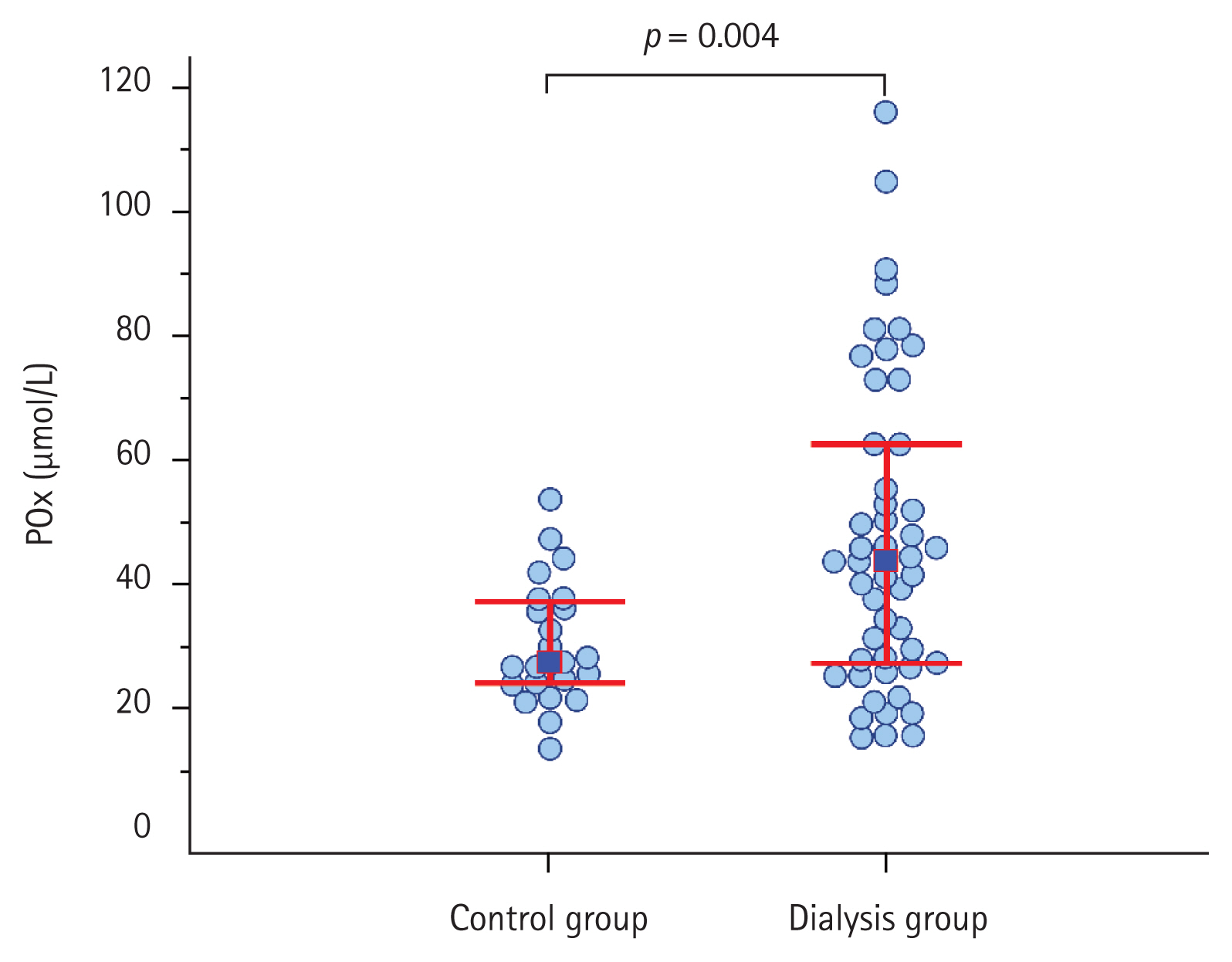
Figure 2
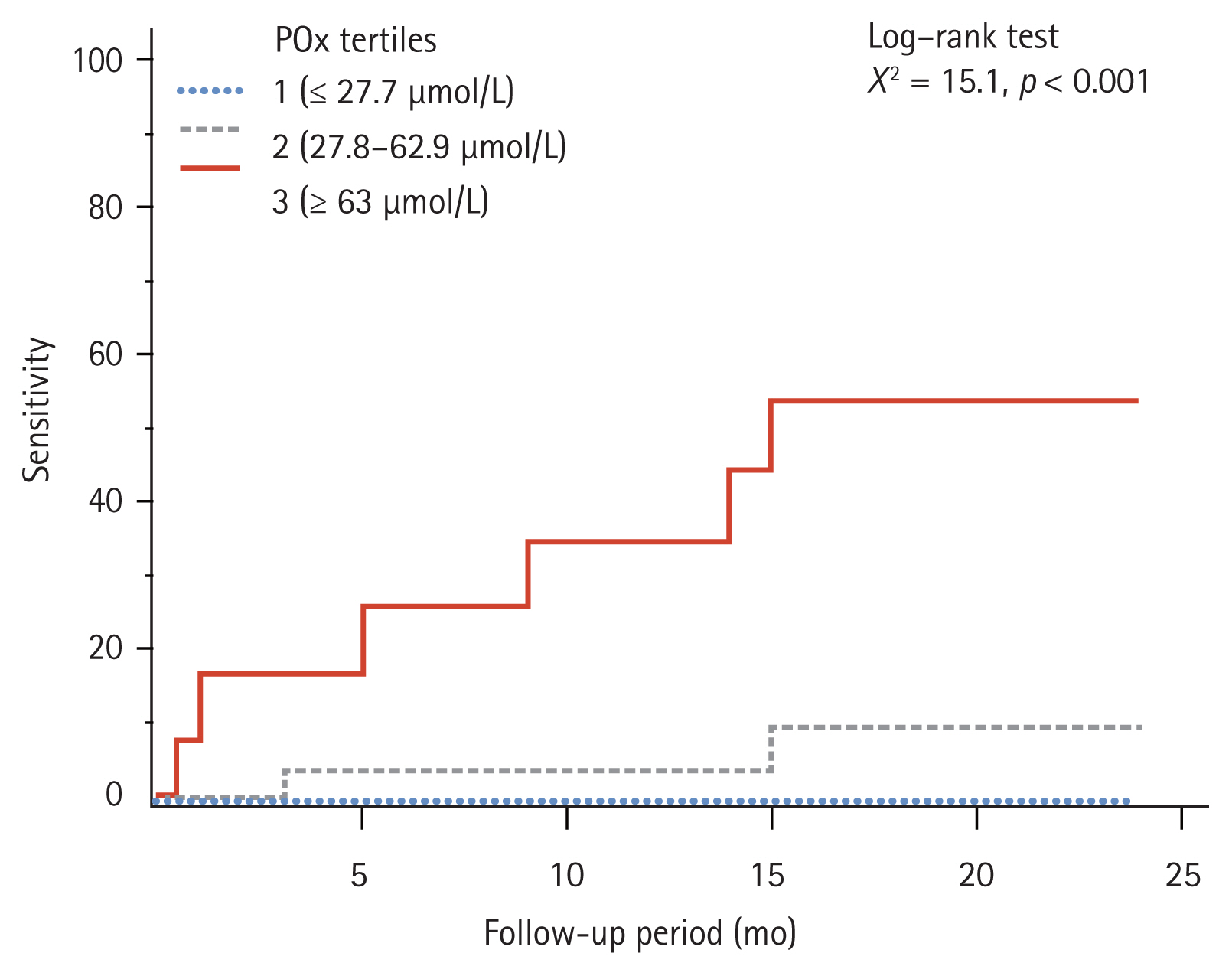
Figure 3
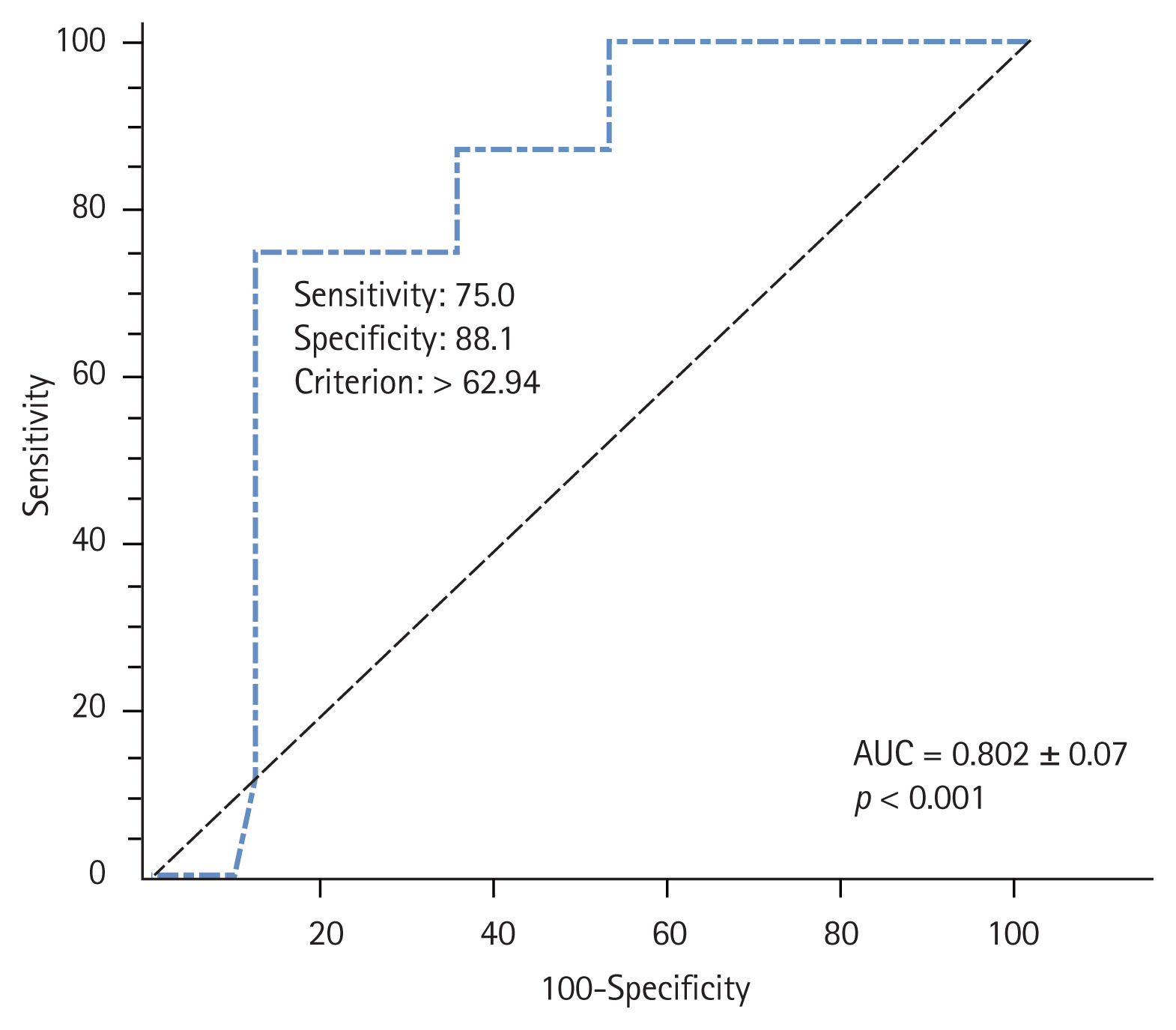
Table 1
Values are presented as number (%), mean ± standard deviation, or median (interquartile range). The values are compared between the groups using the chi-square tests, the Student’s t test and the Mann-Whitney U test as appropriate.
ESRD, end-stage renal disease; RRF, renal residual function; iPTH, intact parathyroid hormone; LDL-C, low-density lipoprotein cholesterol; VLDL-C, very-low-density lipoprotein cholesterol; HDL-C, high-density lipoprotein cholesterol; AIP, atherogenic index of plasma; CRP, C-reactive protein; TNF-α, tumor necrosis factor-alpha; MCP-1, monocyte chemoattractant protein-1.
Table 2
| Variable | POx concentration in the ESRD patients | p value | ||
|---|---|---|---|---|
| Tertile 1 (≤ 27.7 μmol/L) (n = 13) | Tertile 2 (27.8–62.9 μmol/L) (n = 25) | Tertile 3 (≥ 63 μmol/L) (n = 12) | ||
| Lipid profile parameters | ||||
| Total cholesterol, mmol/L | 5.2 (4.2–5.7) | 5.07 (4.4–5.5) | 6.6 (5.9–6.9) | 0.052 |
| Triglycerides, mmol/L | 1.28 (0.87–2.02)c | 1.42 (1.08–1.84)c | 2.8 (1.9–3.1)a,b | 0.002 |
| LDL-C, mmol/L | 3.1 (1.7–3.8) | 2.7 (2.2–3.3) | 3.5 (2.4–3.7) | 0.196 |
| VLDL-C, mmol/L | 0.51 (0.35–0.69)c | 0.64 (0.43–0.88)c | 0.94 (0.63–1.2)a,b | 0.022 |
| HDL-C, mmol/L | 1.44 (1.12–1.66)c | 1.31 (1.2–1.61)c | 1.01 (0.97–1.14)a,b | 0.007 |
| AIP | 2.9 (2.1–3.3)c | 3.1 (2.2–4.0)c | 4.1 (3.7–4.4)a,b | 0.026 |
| Pro-inflammatory markers | ||||
| CRP, mg/L | 7.6 (4.1–11.4) | 11.6 (4.8–15.1) | 11.7 (8.4–14.9) | 0.355 |
| Interleukin 6, pg/mL | 1.1 (0–5.8)c | 1.9 (0.5–4.7)c | 15.9 (8.8–21.1)a,b | 0.006 |
| TNF-α, pg/mL | 2.1 (1.1–4.3)b | 0.16 (0–0.8)a,c | 1.8 (0.5–2.8)b | < 0.001 |
| MCP-1, pg/mL | 254 (219.6–300)b,c | 331.2 (289.5–361.5)a,c | 402 (300–503.8)a,b | 0.001 |
Values are presented as median (interquartile range) and compared between the groups using the Kruskal-Wallis test.
POx, plasma oxalic acid; ESRD, end-stage renal disease; LDL-C, low-density lipoprotein cholesterol; VLDL-C, very-low-density lipoprotein cholesterol; HDL-C, high-density lipoprotein cholesterol; AIP, atherogenic index of plasma; CRP, C-reactive protein; TNF-α, tumor necrosis factor-alpha; MCP-1, monocyte chemoattractant protein-1.
Table 3
| Variable | Value | SD | Wald χ2 | p value | HR (95% CI) |
|---|---|---|---|---|---|
| Unadjusted | 0.028 | 0.012 | 5.808 | 0.016 | 1.03 (1.005–1.05) |
| Model 1 | 0.074 | 0.023 | 10.732 | 0.001 | 1.1 (1.46–1.15) |
| Model 2 | 0.131 | 0.037 | 12.642 | < 0.001 | 1.14 (1.07–1.22) |
Model 1 was adjusted for age, sex, and dialysis modality; Model 2 was additionally adjusted for cardiovascular disease risk factors, including diabetic status, systolic blood pressure, body mass index, serum uric acid, and variables that were statistically significant in the univariate analysis (hemoglobin, triglycerides, interleukin-6).



 PDF Links
PDF Links PubReader
PubReader ePub Link
ePub Link Full text via DOI
Full text via DOI Download Citation
Download Citation Supplement 1
Supplement 1 Print
Print



