 |
 |
| Korean J Intern Med > Volume 37(2); 2022 > Article |
|
Abstract
Background/Aims
Recent advances in the understanding of the pathophysiology of myeloproliferative neoplasms (MPN) were not paralleled with advances in treatment options; thus many questions regarding optimal MPN management remain unanswered. Here, we report the results of descriptive survey study of Korean MPN patients and their attending physicians.
Methods
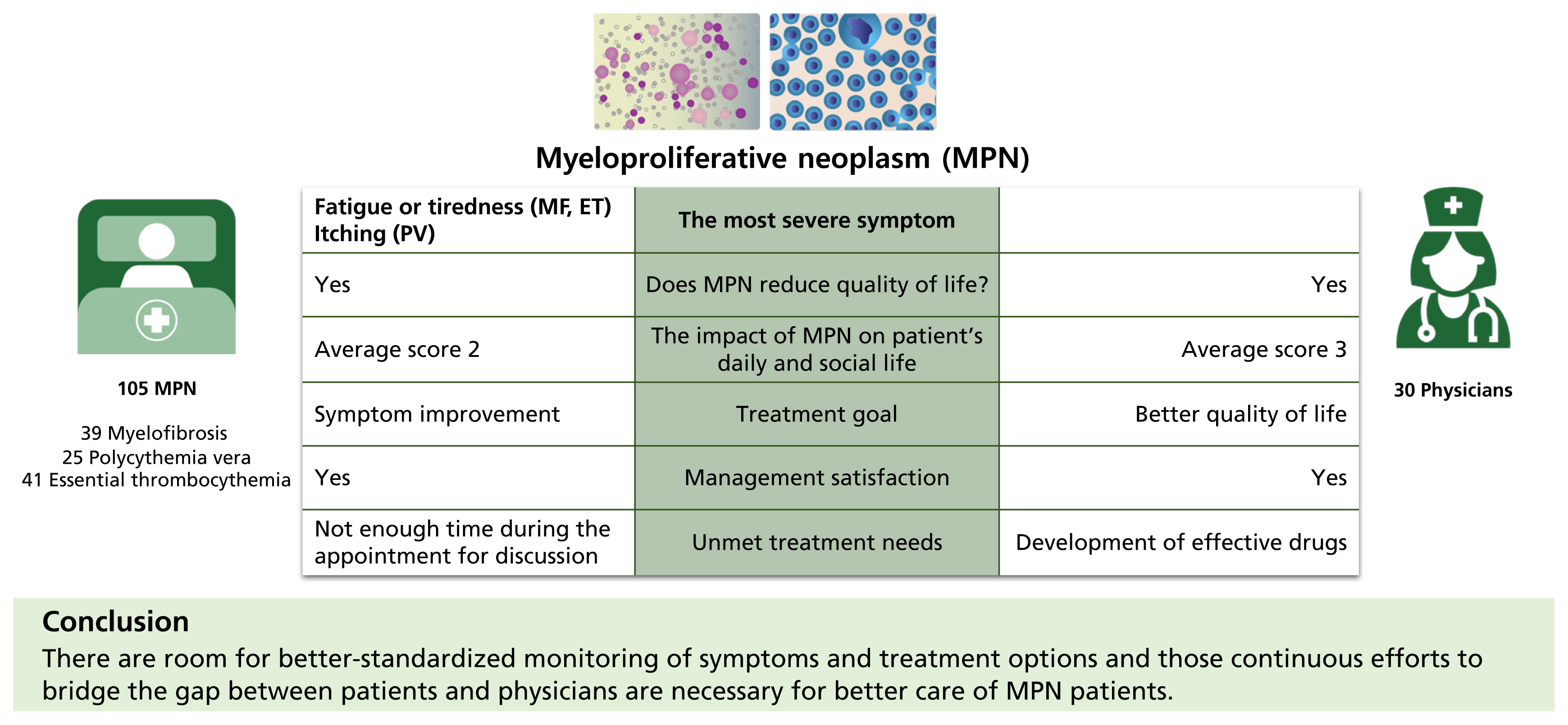
A total of 105 Korean patients (myelofibrosis [MF], 39; polycythemia vera [PV], 25; essential thrombocythemia [ET], 41) and 30 physicians completed the Landmark Health Survey, then data from the survey were analyzed.
Results
Among the MPN-Symptom Assessment Form symptoms, the most severe symptom reported was ‘fatigue or tiredness’ in MF and ET patients and ‘itching’ in PV patients. The majority of the patients agreed that MPN reduced their quality of life (QoL). Interestingly, physicians gave higher scores regarding the impact of MPN on patient’s daily and social life compared to patients themselves. For patients, the most important treatment goal was symptom improvement regardless of MPN subtype, while for physicians the highest priority for treatment was better QoL regardless of MPN subtype. Generally, both patients and physicians were satisfied with the overall treatment/management of MPN and communications. However, many patients felt there was not enough time during the appointment for discussion, while many physicians felt they lacked effective drugs to offer to their patients.
BCR-ABL negative myeloproliferative neoplasms (MPN) represent a heterogeneous group of clonal hematopoietic disorders and are comprised of myelofibrosis (MF), polycythemia vera (PV), and essential thrombocythemia (ET). Most MPN share relatively “indolent” clinical courses, but many patients experience compromised quality of life (QoL) of varying degrees due to MPN associated organomegaly, cytopenia, and a broad range of constitutional symptoms [1,2]. The identification of distinct recurrent mutations, namely JAK2 V617F [3], has led to a better understanding of the underlying pathophysiology. However, such advances in knowledge were not paralleled with advances in treatment options, thus many questions regarding optimal MPN disease burden management remain unanswered. All in all, with an expected increment in both incidence and prevalence, MPN poses a cumulative threat to public health including but not limited to substantial economic and social burdens.
A descriptive survey study provides an important set of information on a patient’s perception and experience of a disease, which assists in recognizing and resolving unmet medical needs. Resonating such sentiment, MPN Landmark Health Survey was conducted in the United States [4,5] and other countries [6] to comprehensively evaluate the impact of MPN on patients as well as on attending physicians. H ere, we report the experience of Korean MPN patients and their attending physicians.
The Landmark Health Survey was an international, cross-sectional survey of patients diagnosed with MPN and treating physicians conducted from October 2018 to December 2018 in six countries (South Korea, China, Russia, Saudi Arabia, Taiwan, and Turkey). The patient and physician surveys included 62 and 47 questions, respectively, were administered online. All respondents provided consent to the survey. The survey required approximately 30 minutes to complete and consisted of six domains including demographics, disease characteristics, the burden of disease, treatment and drug utilization, attitudes towards disease and treatment, and the physician-patient relationship. MPN symptoms were rated score range from 0 (not severe at all) to 10 (worst imaginable). We used data of 43 patients and 30 physicians from South Korea for analysis. This part of the study was approved by a central ethics review board, Salus Institutional Review Board (IRB).
Then, we additionally recruited 64 patients from six medical centers in South Korea from May 2020 to August 2020. This study was approved by the Institutional Review Boards each participating hospital: Korea University Guro Hospital (IRB number 2020GR0162); Seoul National University Bundang Hospital (IRB number B-2006-619-402); Samsung Medical Center (IRB number 2020-02-170); Seoul National University Hospital (IRB number H-2003-081-1109); Seoul St. Mary’s Hospital (IRB number KC20QSDI0301); Asan Medical Center (IRB number 2020-0385). Physicians at each center recruited patients during normal consultations and provided patients with the same survey in its paper form. The patients returned the completed survey via mail to ensure respondent anonymity. After excluding two patients for lack of data on their diagnosis, data from 62 patients were finally used.
For both parts of the survey, patients diagnosed with MF, PV, or ET who were ≥ 19 years of age were deemed eligible. Physicians who were actively involved in managing MPN patients, defined as ≥ 2 MF patients, ≥ 2 PV patients, ≥ 4 ET patients seen in the last 12 months, were recruited to take the survey. In the end, data from 105 patients (39 MF, 25 PV, 41 ET) and 30 physicians were used for this study (Supplementary Fig. 1).
Data from the survey were transferred to a single electronic database. All statistical analyses were performed by using the software package SAS version 9.4 software (SAS Institute Inc., Cary, NC, USA). Analyses used descriptive statistics. For numerical variables, median (range), and mean ± standard deviation are presented. For categorical values, the number and percentage of subjects in each category are shown. The Student’s t test was used to compare continuous variables when the two groups showed a normal distribution, and otherwise, the Wilcoxon rank-sum test was used. For categorical variables, the chi-square test, the Fisher’s exact test and the Kruskal-Wallis test were used.
Symptom severity was assessed by quartiles (Q1–Q4). On a scale of 0 to 140, symptom severity quartiles were determined post-data collection to include a similar number of patients in each quartile. The quartiles were defined as follows: quartile 1, 0–12; quartile 2, 13–22; quartile 3, 23–43; and quartile 4, 44–140. Prognostic risk scores were calculated based on information provided by respondents. The scores were generated using published scoring systems for MF (International Prognostic Scoring System; IPSS) [7], PV [8], and ET [9].
Baseline patient demographics are presented in Table 1. The median age at MPN diagnosis was similar for MF (61 years) and PV patients (63 years), but ET patients were significantly younger (55 years, p = 0.0025). The median disease duration was 4 years, regardless of MPN subtype. In retrospect, the majority of the MF patients reported that they experienced MPN-related symptoms for more than 6 months before diagnosis. In contrast, many of the PV (45.45%) and ET (40.00%) patients answered that their MPN-related symptoms were present for less than 6 months before diagnosis. Per prognostic risk group, patients with intermediate-risk were predominant. There were 18 (17.82%) patients who were unaware of their risk, of whom ET was most prevalent.
Baseline physician characteristics are shown in Supplementary Table 1. A total of 30 physicians with a background in hemato-oncology participated, and all worked in either university or teaching hospitals. Most of the physicians were qualified to practice between 2005 and 2015 (56.67%). Overall, physicians reported they saw a higher number of ET patients than MF or PV patients (MF, 5.07 patients; PV, 5.43 patients; ET, 6.53 patients).
Supplementary Table 2 represents the symptoms patients experienced within the last 12 months. Overall, fatigue was the most reported symptom, especially in MF and ET patients (mean severity score: overall, 4.63 ± 2.39; MF, 4.99 ± 2.36; ET, 5.00 ± 2.26). In PV patients, itching (pruritus) was the most common and severe symptom listed in MPN-Symptom Assessment Form (MPN-SAF). Of note, there was no symptom with an MPN severity score of more than 5. MF patients had the highest mean score of MPN-SAF Total Symptom Score (TSS) followed by PV and ET patients (MF, 16.84; PV, 14.87; ET, 13.59). Specifics of most often experienced symptoms and most severe symptoms are shown in Supplementary Figs. 2 and 3.
Regardless of MPN subtypes, many patients reported MPN related symptoms reduced their QoL. This phenomenon was most prominently noted in MF patients followed by PV and ET (MF, 94%; PV; 68%; ET, 63%, p = 0.0004) (Supplementary Table 3). Most patients agreed that ‘MPN related symptoms reduce my QoL,’ and ‘MPN may progress to a more serious condition’ regardless of their diagnosis.
Supplementary Table 4 shows caregiver reliance about MPN disease burden. One-third of MF patients needed a caregiver (rarely, 15.79%; sometimes, 5.26%; often, 10.53%), while 20% of ET and only 12% PV patients required assistance. Of those who reported they needed a caregiver, approximately 61% said their spouse was their primary caregiver. The most common tasks patients required help were transportation (75%), homemaking (60%), and companionship (40%). The patients required a caregiver for an average of 14.45 ± 17.13 hours per 7 days.
Table 2 shows the difference in patients’ and physicians’ perceptions regarding the impact MPN has on their daily and social lives. Generally, physicians gave higher scores in comparison to patients.
As shown in Fig. 1, for patients the most important treatment goal was symptom improvement regardless of MPN subtype (MF, 71.79%; PV, 72%; and ET, 58.54%). This was also independent of prognostic risk score (high, 60.00%; intermediate, 72.09%; low, 67.74%) (Fig. 1D) and symptom severity (Q1, 61.90%; Q2, 76.67%; Q3, 59.26%; Q4, 66.67%) (Fig. 1E). Of note, PV patients were most interested in healthy blood count, while ET patients were most interested in preventing vascular/thrombotic events.
On the other hand, for physicians, the highest priority for treatment was better QoL regardless of MPN subtype. The second most important treatment goal differed according to the MPN subgroup: for MF it was slow progression; for ET preventing vascular/thrombotic events, and for PV symptom improvement.
The symptom patients would most like to resolve was fatigue or tiredness for MF (66.67%) and ET (46.34%) and itching (pruritus) for PV (44.00%). Physicians thought symptoms that patients most like to resolve were fatigue or tiredness for MF (83.33%) and PV (20.00%) and blood clots for ET (30.00%) (Fig. 1F–1H).
The overall treatment is shown in Supplementary Table 5. Ruxolitinib was used in 64.1% of the MF patients, 4.88% of ET patients, and none in PV. Three patients had an experience of being enrolled in a clinical trial. There were few patients dissatisfied with the treatment they were receiving, but all physicians reported that they were satisfied with the therapy they were providing (Fig. 2A).
Most patients were satisfied with patient-physician communication, as shown Figs. 2B, 3A and 3B. More specifically, patients reported that doctors proactively ask how they feel (40%) or ask them about the most important symptoms on the doctor’s assessment of patient symptoms (37.78%) (Table 3). Interestingly, while most physicians reported that they were satisfied with patient-physician communication, physicians reported that they “Have patient fill out some type of symptom checklist and review each symptom” instead of proactively asking their patients about their symptoms.
The perception of unmet treatment needs by physicians was different per MPN subgroup. Physicians responded that the development of effective drugs/therapy should be most promptly addressed for MF and ET, while the cure is the ultimate goal for PV (Fig. 2C). Even so, most patients felt informed about new treatment options and involved in their treatment decision-making process (Fig. 3C and 3D).
Discordance between patient and physician perception of disease is unfortunately not unusual in the medical field, and especially true for chronic illnesses [10,11]. MPN is interesting in this regard because although they are “neoplastic,” in most cases the disease is associated with a long clinical course, and the main treatment goal is heavily geared towards “symptom relief” rather than “cure.” In such a scenario, an accurate understanding of the disease burden and treatment goals is important for the optimization of patient care and subsequently patient outcomes. The importance of our study lies in that we investigated the discrepancy in experience and expectations between Korean MPN patients versus physicians.
The vast majority of the patients reported that their risk score was either low (29.70%) or intermediate (42.57%) (Table 1). This can explain the generally lower MPN-SAF TSS in our patients (Supplementary Table 2) compared to those from the United States [4]. It is noteworthy that 17.82% of the patients did not know their risk score, indicating there is room for better patient education about their disease. It is also important to recognize that lower MPN-SAF TSS did not mean there were no impediments caused by the disease, and 76.19% of all patients either strongly agreed or somewhat agreed that MPN related symptoms were reducing their QoL (Supplementary Table 3). Such gap suggests that perhaps patients are living with symptoms that they do not fully recognize as being related to MPN. This again suggests better patient education on the physician’s part but also highlights the importance of regular symptom assessments for treatment decision guides.
The most prominent discordance between patients and physicians concerned treatment goals. While physicians answered better QoL is the main treatment goal for all MPN patients regardless of subtype, patients reported symptom improvement was their main treatment goal regardless of MPN subtype (Fig. 1). Such differences might have resulted from the difference in understanding the underlying pathophysiology of the disease. As for which symptom requires most urgent attention, physicians thought their patients were most hampered by fatigues/tiredness, but the symptom patients would most like to resolve differed among MPN subtypes. Interestingly most physicians strongly agreed that QoL is compromised by symptoms for MF patients, but not as much for PV or ET patients. Somewhat biased perception of physicians probably stems from previous reports [12–14]. Coinciding with the general understanding of MPN prognosis, physicians responded that the development of effective drugs/therapy should be most promptly addressed for MF and ET, while the cure is the ultimate goal for PV (Fig. 2C). It is important to move beyond such biases and listen to the patients for improved patient satisfaction.
Even so, most patients were satisfied with patient-physician communications (Fig. 2B). Notably, physicians were less satisfied with their communications with patients. Especially, physicians and patients felt differently about the treatment decision-making process. Most patients felt in volved in the treatment decision-making process (Fig. 3), but approximately half of the physicians felt either it was unnecessary to involve the patients or that treatment decision should physician-directed (Fig. 3D and 3E). Patients also reported that physicians seemed more interested in discussing blood counts rather than their symptoms (Fig. 3F), and thus there was not enough time to talk about their symptoms (Fig. 3G). Whether patient-centric communications lead to better patient adherence and treatment outcomes is yet to be seen in MPN settings, but our findings highlight the need for continuous efforts to bridge the gap between patients and physicians.
Another interesting aspect of our study is the vicarious exploration of how cultural factors impact the clinical encounter between healthcare providers and patients. We saw that more Western physicians proactively asks how patient is feeling and their symptoms [5] compared to Korean doctors, whereas treatment goals were similar across the globe [4,6]. Perhaps related to the difference in communication styles, more Western patients felt satisfied with physician management (very satisfied Western MF patients 64.3% vs. Korean MF patients 48.7%; PV 60.5% vs. 60.0%; ET 58.0% vs. 33.3%) and communications (very satisfied Western MF patients 66.2% vs. Korean patients 38.46%; PV 57.1% vs. 76.0%; ET 54.9% vs. 38.5%) compared to Korean patients [5]. Since it has been suggested that patient’s cultural approaches to disease etiology and illness affect the patient’s care-seeking behaviors, treatment choices and compliance [15], a culturally sensitive approach to chronic disease like MPN may lead to patient adherence and improved health outcomes.
As with previous studies reporting the results of the Landmark Health Survey [4–6,16], major pitfalls of this report come from the nature of the study. First, because this survey heavily relied on patient’s retrospective recollection and awareness of their disease and treatment, some differences can be due to patient error. Especially because responses were not matched between a physician and the specific patient under his/her care, data comparison and interpretation can be difficult. Secondly, there were only 30 physicians, in comparison to 105 patients, who participated in this study. All physicians worked in either university or teaching hospitals, thus there may have been a selection bias.
In conclusion, our study provides comprehensive insights into the impacts of MPN on both patients and physicians. Our study suggests that there are room for better monitoring of symptoms and patient-physician communications. In particular, continuous efforts to close the gap between patients and physicians regarding treatment goals and treatment decisions are necessary for improved overall satisfaction.
1. We investigated the discrepancy in experience and expectations between Korean myeloproliferative neoplasm patients versus physicians.
2. Continuous efforts to close the gap between patients and physicians regarding treatment goals and treatment decisions are necessary for improved overall satisfaction.
Conflict of Interest
Jiwon Park is a medial liason at Novartis Korea, Seoul, South Korea. The authors thank Hyeseon Lee of Dream CIS Ltd. for providing medical writing support and editorial support for this manuscript, which was funded by Novartis Korea, Seoul, South Korea under Good Publication Practice (GPP3) guidelines ( http://www.ismpp.org/gpp3).
Figure 1
Most important treatment goals (A–E) and symptoms patients most like to resolve (F–H). Most important treatment goals (A) for myelofibrosis, (B) for polycythemia vera, (C) for essential thrombocythemia, (D) according to myeloproliferative neoplasm (MPN) risk score, (E) according to MPN symptom severity. Symptoms patients most like to resolve (F) for myelofibrosis, (G) for polycythemia vera, (H) for essential thrombocythemia.
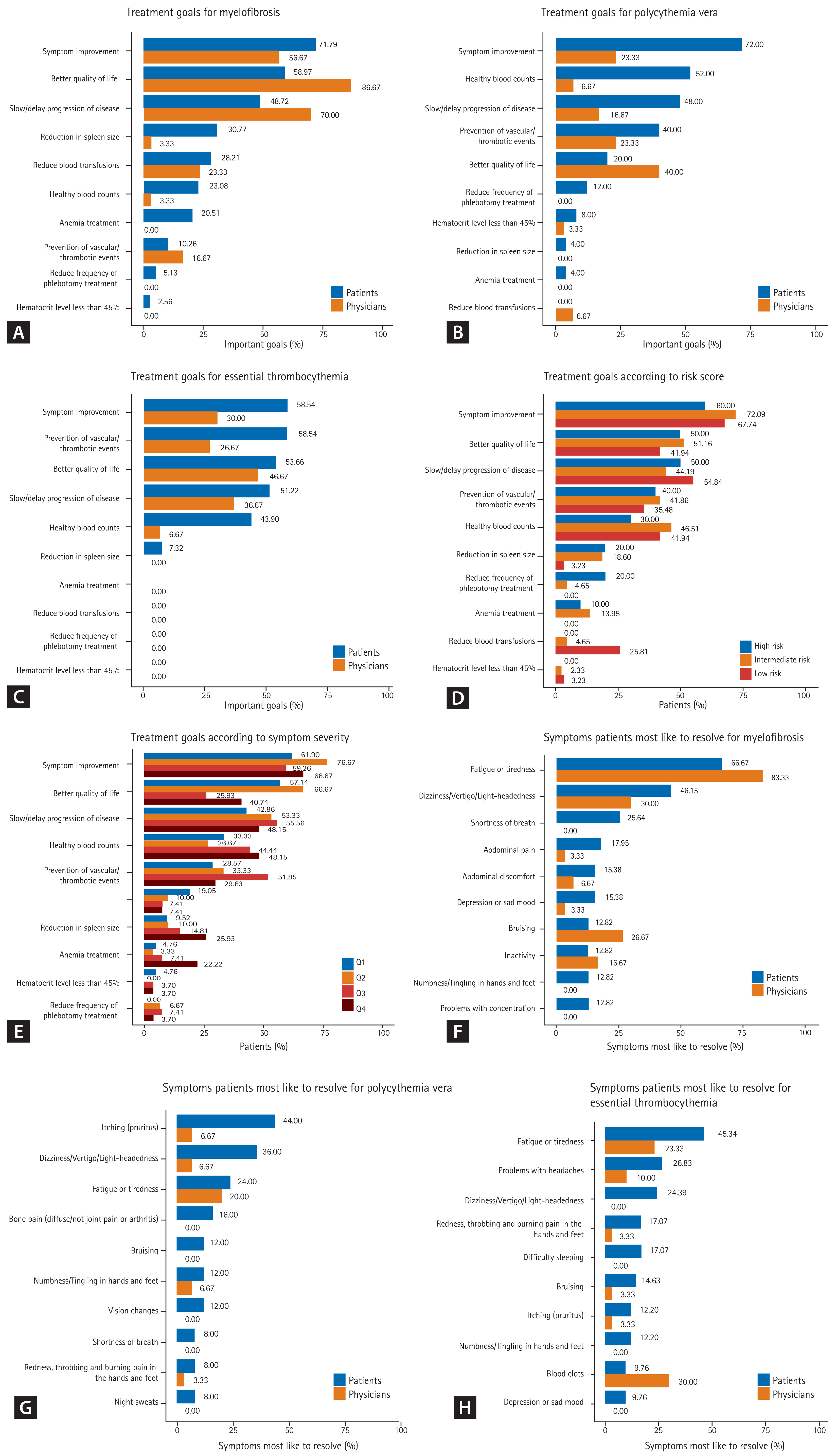
Figure 2
Satisfaction regarding communication and treatment. (A) Overall treatment and management of myeloproliferative neoplasm, (B) patient-physician communications, (C) unmet medical needs from physicians’ point of view. MF, myelofibrosis; PV, polycythemia vera; ET, essential thrombocythemia.
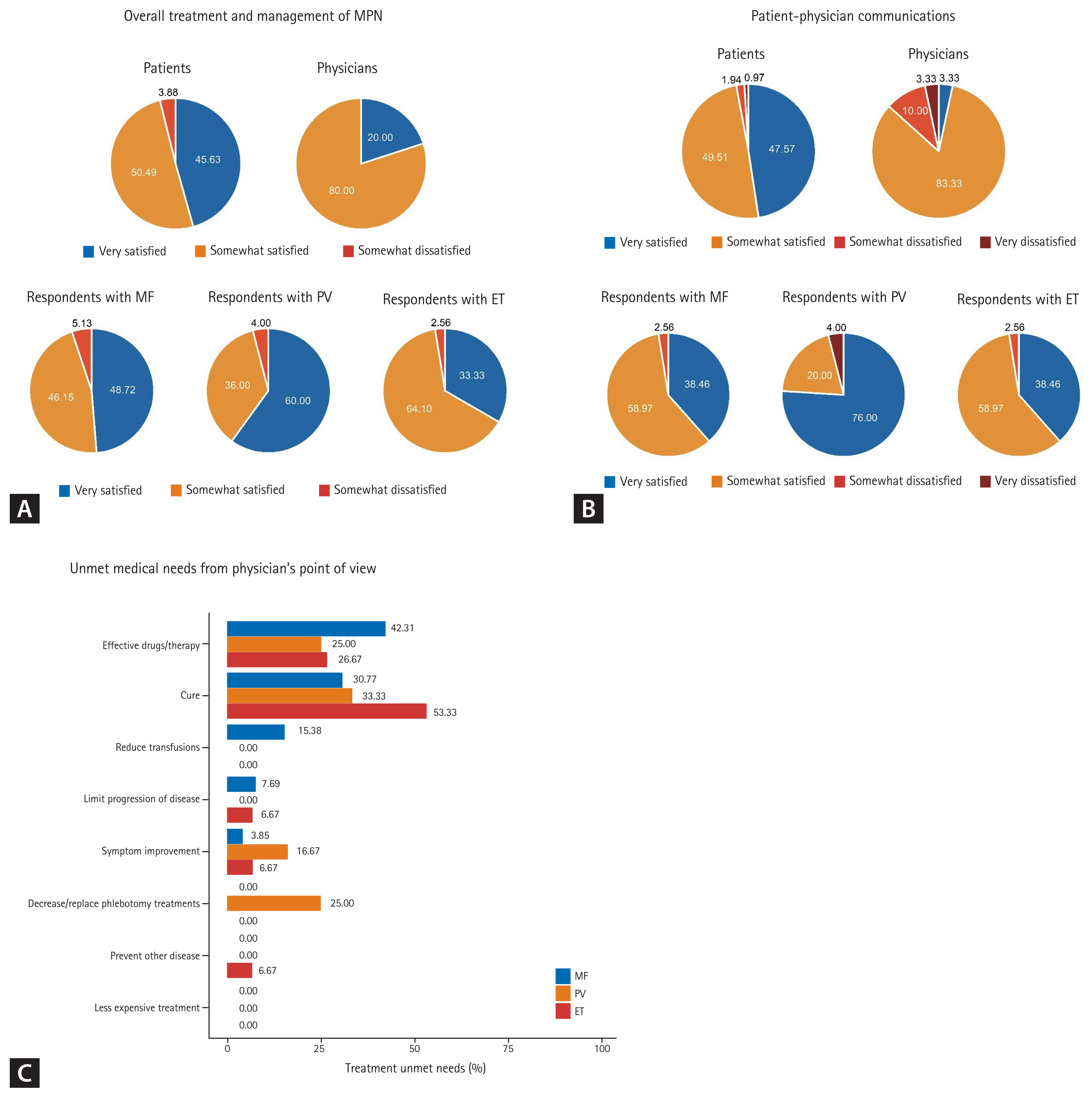
Figure 3
Patients versus physicians on communications regarding treatment. (A) Doctor listens to patient’s concerns and address their questions. (B) Doctor asks patient about their symptoms at every appointment. (C) Doctor keeps patient informed about new treatment options. (D) Doctor involves patient in decisions about their treatment. (E) Doctor has created a treatment plan or goals for therapy for patients. (F) Doctor seems more interested in discussing blood counts. (G) There’s not enough time during the appointment to discuss all patient’s symptoms.

Table 1
Patient characteristics
Table 2
Impact of myeloproliferative neoplasms related symptoms on life, perceived by patients versus physicians
| Scorea | MF | PV | ET | All |
|---|---|---|---|---|
| No. of patients | 39 | 25 | 41 | 105 |
| My condition has interfered with my daily activities | 2 (1–5) | 3 (1–5) | 2 (1–4) | 2 (1–5) |
| My condition has interfered with my family or social life | 2 (1–5) | 1 (1–5) | 2 (1–5) | 2 (1–5) |
| My condition has interfered with my sex life | 2 (1–5) | 1 (1–5) | 2 (1–5) | 2 (1–5) |
| Pain and discomfort have caused me to limit my activities | 2 (1–5) | 2 (1–4) | 2 (1–5) | 2 (1–5) |
| My condition has interfered with my relationship with my caregiver | 1.5 (1–5) | 1 (1–5) | 1 (1–3) | 1 (1–5) |
| No. of physicians | 30 | 30 | 30 | 90 |
| Their condition has interfered with their daily activities | 3 (2–5) | 3 (2–4) | 3 (2–4) | 3 (2–5) |
| Their condition has interfered with their family or social life | 3 (2–4) | 3 (2–4) | 2 (2–4) | 3 (2–4) |
| Their condition has interfered with their sex life | 3 (2–4) | 3 (2–3) | 3 (1–3) | 3 (1–4) |
| Pain and discomfort have caused them to limit their activities | 3 (1–4) | 2 (2–3) | 2 (2–3) | 3 (1–4) |
| Their condition has interfered with their relationship with their caregiver (If they have a caregiver) | 2 (1–3) | 2 (1–3) | 2 (1–3) | 2 (1–3) |
Table 3
Patient and physician respondent perspectives on communications
REFERENCES
1. Emanuel RM, Dueck AC, Geyer HL, et al. Myeloproliferative neoplasm (MPN) symptom assessment form total symptom score: prospective international assessment of an abbreviated symptom burden scoring system among patients with MPNs. J Clin Oncol 2012;30:4098–4103.



2. Scherber R, Dueck AC, Johansson P, et al. The Myeloproliferative Neoplasm Symptom Assessment Form (MPN-SAF): international prospective validation and reliability trial in 402 patients. Blood 2011;118:401–408.


3. Kralovics R, Passamonti F, Buser AS, et al. A gain-of-function mutation of JAK2 in myeloproliferative disorders. N Engl J Med 2005;352:1779–1790.


4. Mesa R, Miller CB, Thyne M, et al. Myeloproliferative neoplasms (MPNs) have a significant impact on patients’ overall health and productivity: the MPN Landmark survey. BMC Cancer 2016;16:167.



5. Mesa RA, Miller CB, Thyne M, et al. Differences in treatment goals and perception of symptom burden between patients with myeloproliferative neoplasms (MPNs) and hematologists/oncologists in the United States: findings from the MPN Landmark survey. Cancer 2017;123:449–458.


6. Harrison CN, Koschmieder S, Foltz L, et al. The impact of myeloproliferative neoplasms (MPNs) on patient quality of life and productivity: results from the international MPN Landmark survey. Ann Hematol 2017;96:1653–1665.



7. Cervantes F, Dupriez B, Pereira A, et al. New prognostic scoring system for primary myelofibrosis based on a study of the International Working Group for Myelofibrosis Research and Treatment. Blood 2009;113:2895–2901.


8. Tefferi A, Rumi E, Finazzi G, et al. Survival and prognosis among 1545 patients with contemporary polycythemia vera: an international study. Leukemia 2013;27:1874–1881.



9. Passamonti F, Thiele J, Girodon F, et al. A prognostic model to predict survival in 867 World Health Organization-defined essential thrombocythemia at diagnosis: a study by the International Working Group on Myelofibrosis Research and Treatment. Blood 2012;120:1197–1201.


10. Alexander JA, Hearld LR, Mittler JN, Harvey J. Patient-physician role relationships and patient activation among individuals with chronic illness. Health Serv Res 2012;47(3 Pt 1):1201–1223.


11. Alexander J, Hearld L, Mittler JN. Patient-physician role relationships and patient activation: the moderating effects of race and ethnicity. Med Care Res Rev 2014;71:472–495.


12. Mesa RA, Niblack J, Wadleigh M, et al. The burden of fatigue and quality of life in myeloproliferative disorders (MPDs): an international Internet-based survey of 1179 MPD patients. Cancer 2007;109:68–76.


13. Scherber RM, Kosiorek HE, Senyak Z, et al. Comprehensively understanding fatigue in patients with myeloproliferative neoplasms. Cancer 2016;122:477–485.


- TOOLS



 PDF Links
PDF Links PubReader
PubReader ePub Link
ePub Link Full text via DOI
Full text via DOI Download Citation
Download Citation Supplement 1
Supplement 1 Print
Print



