 |
 |
| Korean J Intern Med > Volume 40(5); 2025 > Article |
|
Abstract
Background/Aims
Methods
Results
Notes
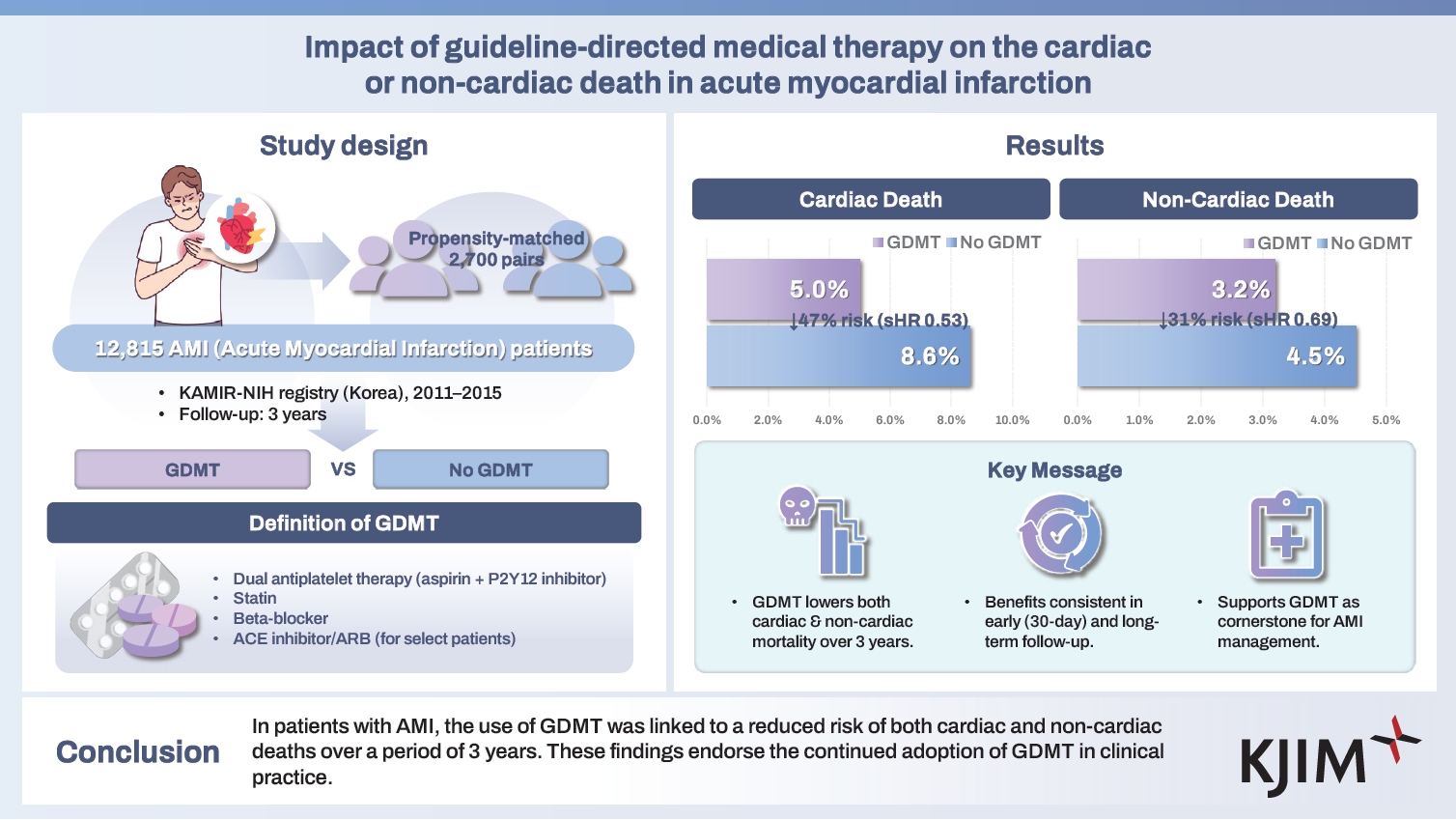
Figure 1.
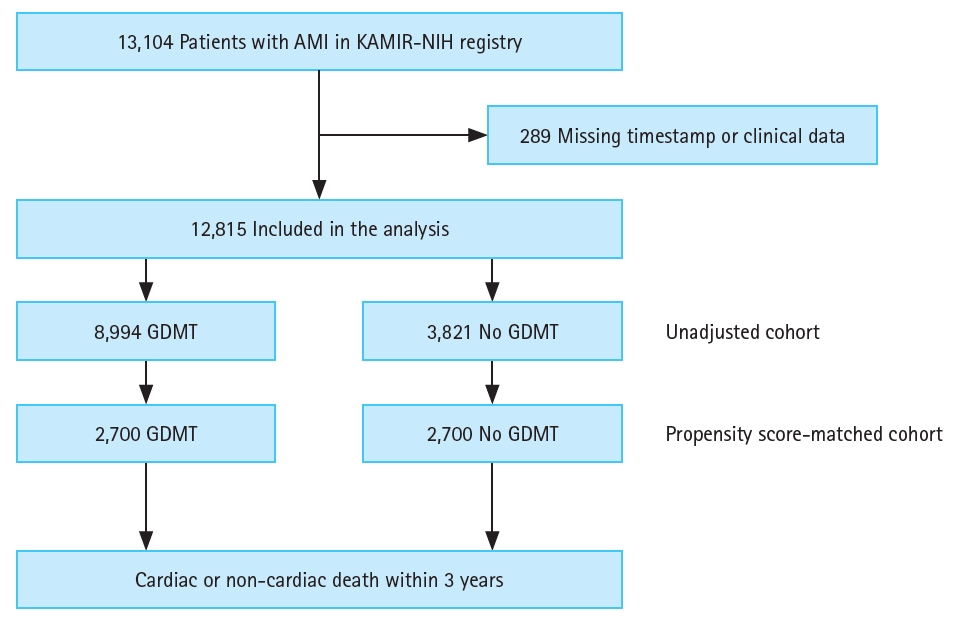
Figure 2.
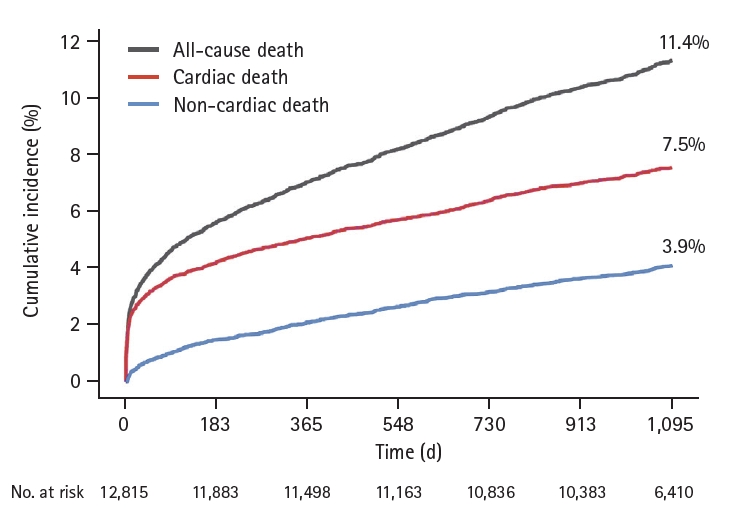
Figure 3.
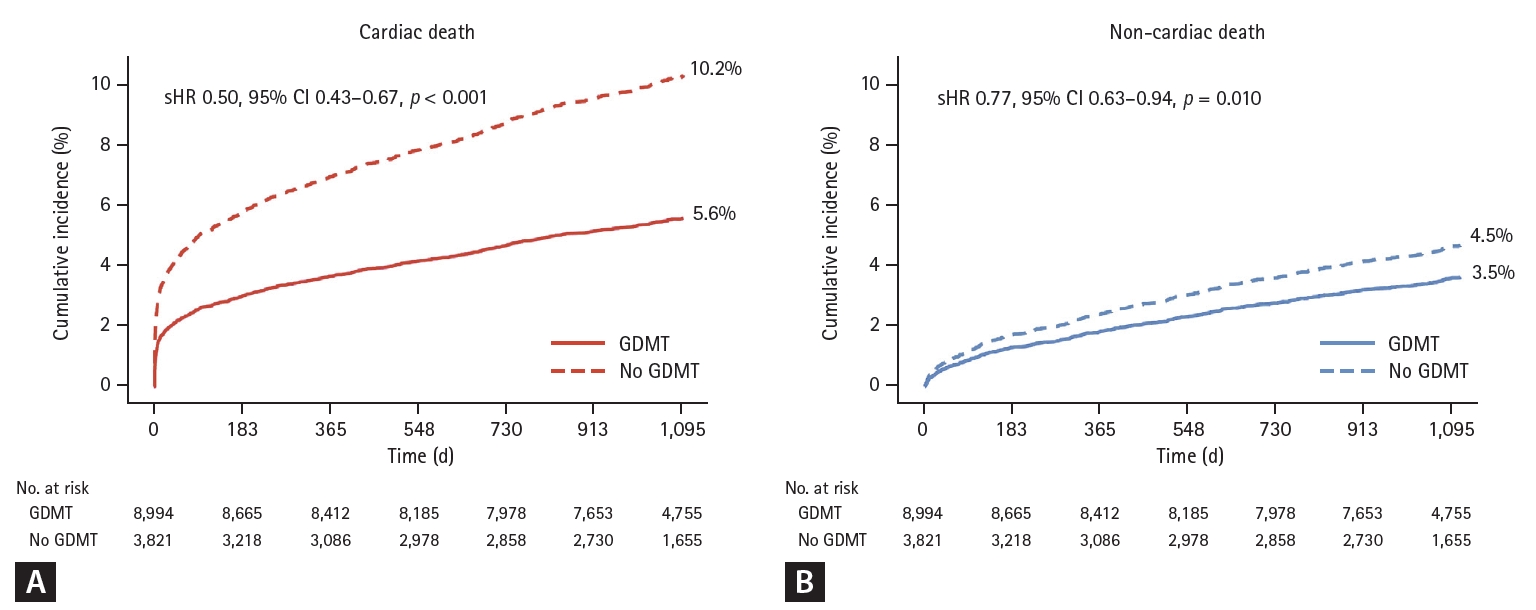
Figure 4.
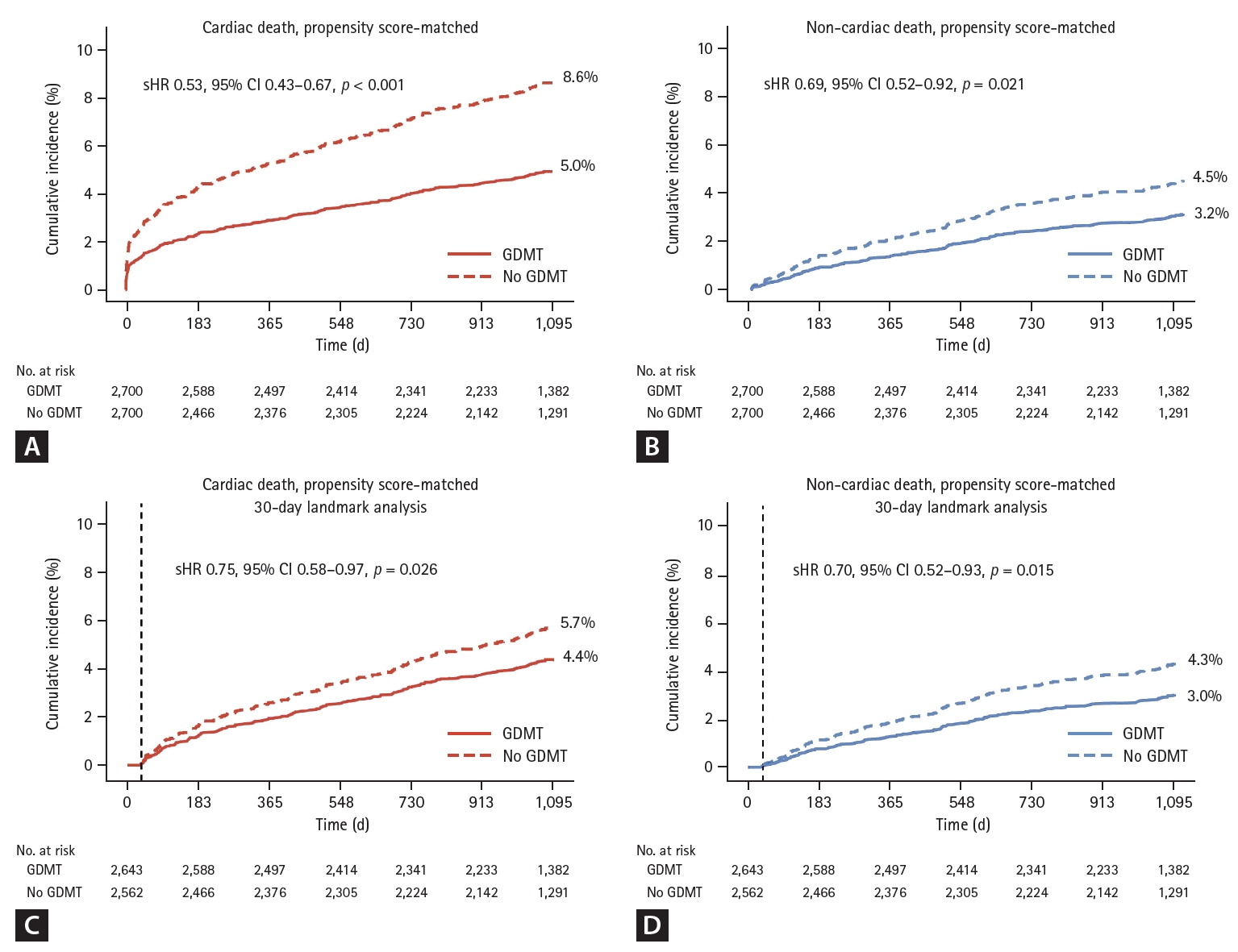
Table 1.
Clinical characteristics of patients with GDMT and those without GDMT are presented for both the entire patient cohort and the propensity score-matched subset. Data are shown as mean ± standard deviation or counts and percentages (%).
GDMT, guideline-directed medical therapy; STEMI, ST-elevation myocardial infarction; LAD, left anterior descending artery; DAPT, dual antiplatelet therapy; SAPT, single antiplatelet therapy; ACEi, angiotensin-converting enzyme inhibitor; ARB, angiotensin receptor blocker; SMD, standardized mean difference.
Table 2.
Table 3.
Data are shown as cumulative incidence (%) or restricted mean time lost (RMTL) (days) with 95% confidence intervals. Both the subdistribution hazard model that incorporates competing risks and the cause-specific hazard model are presented to provide a comprehensive assessment of outcome risks. The proportional hazards assumption was evaluated using the scaled Schoenfeld residuals at a significance level of 0.05 for patients with GDMT and those without GDMT. This assumption was not met in the analysis of all patients or propensity score-matched patients (p < 0.05, both), but it held in 30-day landmark analysis of propensity score-matched patients (p >0.05). To address the discrepancy in the proportional hazards assumption, RMTL was additionally calculated to assess the absolute benefit from GDMT.
GDMT, guideline-directed medical therapy.
REFERENCES
- TOOLS
-
METRICS

-
- 0 Crossref
- 0 Scopus
- 47 View
- 13 Download
- Related articles
-
Pre-hospital delay and emergency medical services in acute myocardial infarction2020 January;35(1)



 PDF Links
PDF Links PubReader
PubReader ePub Link
ePub Link Full text via DOI
Full text via DOI Download Citation
Download Citation Supplement figure 1
Supplement figure 1 Print
Print


